Risks of pregnancy and childbirth with obesity
11.06.2020
The overall weight gain during pregnancy shows too much variation between women in their daily lives or their pregnancies. About 30% of women of childbearing age are obese . Obesity is divided into four stages (according to BMI - body mass index):
- first degree - from 10 to 30% of a woman’s normal weight;
- second degree - from 30 to 50% of a woman’s normal weight;
- third degree - from 50 to 100% of a woman’s normal weight;
- class four - more than 100% above a woman's normal weight.
During pregnancy , a pregnant woman's weight increases by an average of 12-13 kilograms, and at the same time the body shape changes. The average weekly weight gain is about 300 grams. Healthy women increase their weight by an average of 17-20%. Weight gain occurs from the growing fetus, its appendages, increased fluid retention, increased blood breast enlargement and the accumulation of fat and protein reserves. During pregnancy , appetite and food intake increase. Some taste preferences also change.
Pregnancy is a condition that usually leads to a change in carbohydrate tolerance under the influence of hormones (estrogens, progesterone, placental lactogen, etc.).
What are the risks for pregnancy for an obese woman?
- Gestational diabetes is 4-6 times more common in obese
- Hypertensive diseases are more common in these women, including preeclampsia (which can be life-threatening!). Hypertension is combined with hyperlipidemia and hyperuricemia, which can lead to damage to the woman’s body
- Digestive complications - more common cholelithiasis ( gallstones )
- Childbirth proceeds tracheally (for a long time) and with a large number of ruptures of the soft birth canal. Bleeding at birth with complex etiology is more common
What are the obesity issues in pregnancy tracking?
Diagnosis associated with the initial diagnosis of pregnancy . This is due to the difficulty of obstetric examination. History is unreliable in most cases, as these women often experience menstrual irregularities, infertility , or amenorrhea.
Diagnostic difficulties are also found in some acute pregnancy , such as placental abruption (placental abruption), complications in the fibroid node, rupture (rupture) of the uterus .
Symptoms are unclear with concomitant acute surgical conditions ( appendicitis , etc.).
Difficult obstetric examination during pregnancy due to the thick anterior abdominal wall. Palpation according to Leopold (one of the methods of examining pregnant women for the presence of pregnancy ) and auscultation (listening) to heart are difficult.
Uterine height , abdominal and uterine are measured incorrectly.
Ultrasound (one of the most important methods of monitoring pregnancy !) in the fetus is not always accurate due to the thick abdominal wall. In early pregnancy, vaginal ultrasound is preferred.
The best way to give birth is difficult to predict. External pelviometry (pelvic measurement) is inaccurate due to the large amount of fat above the designated measurement points.
Internal obstetric examination of the pelvic space is also inaccurate due to the accumulation of fatty tissue, which in turn reduces the pelvic space. X-ray pelviometry is often necessary to assess pelvic size and shape (which are important indicators in determining the delivery method).
Adviсe:
- during pregnancy you should follow a diet ;
- avoid high-calorie foods;
- monitor changes in your body and do not ignore them;
- metabolic disorders such as the onset of gestational diabetes or the development of insulin resistance are being investigated for rapid supplementation.
- treatment is carried out jointly with an endocrinologist;
- delivery should be vaginal (if possible). Caesarean section is performed only for strict indications;
- Obese pregnant women complications through cesarean section than women of normal weight. The more common are infections of the surgical wound, the greater the blood loss, as well as damage to neighboring pelvic organs;
- In the postpartum period, there is a risk of endometritis (inflammation of the lining of the uterus ) and thromboembolic complications;
- After cesarean section, women are recommended early onset and prevention of thromboembolic complications using low molecular weight heparins;
- Antibiotic prophylaxis is mandatory.
Published in Endocrinology Premium Clinic
The dangers of overweight and underweight
In practice, it happens that a pregnant woman can suddenly gain weight, and this is not good. The body, working at this time for two, finds it difficult to adapt to such a sharp increase in body weight, and therefore problems may arise in the gastrointestinal tract, urinary system and heart.
It's even worse for those who gain excess weight beyond normal limits. Such kilograms do not allow organs to function properly. If a malfunction of the kidneys occurs, this will lead to fluid retention in the body, and then a more serious complication, such as gestosis in pregnant women.
A small gain in weight will also not bring anything good. In this case, the baby will lack nutrients and vitamins, which will affect his further development. In the early stages, this can lead to miscarriage.
What causes weight gain during pregnancy?
The bulk of the added weight is the child's weight. On average, the fruit weighs from 3.2 to 3.6 kilograms. But in addition to the child’s weight, the increase is calculated from the following1:
- The increase in blood volume is about 1.3-1.8 kg.
- The weight of fluid in the body increases by 0.9-1.3 kg.
- Another 2.7-3.6 kg are the necessary fat deposits.
- 0.9-1.3 kg accounts for a significant increase in mammary glands.
- The placenta weighs 0.7 kg.
- The uterus increases in weight by 0.9 kg.
As already mentioned, a weight gain of up to 16 kg is normal and should not cause concern to the expectant mother.
Calculation of body mass index in pregnant women
Pregnant women are afraid of gaining a lot of weight and may start following a diet that will not be beneficial for the health of the unborn child.
By calculating your body mass index, you can calculate your rate of increase. To calculate BMI, you need to divide your actual weight (kg) by your height (m) squared. This way you will get the maximum weight that you can gain during pregnancy without harming yourself and the fetus.
If you have any doubts or concerns, consult your doctor. The child will develop normally and feel good if the growth of body weight occurs smoothly.
If you are just planning a pregnancy, then immediately calculate how many kilograms you can gain safely based on your BMI.
- If your BMI is less than 18.5, you can safely gain up to 18 kg during pregnancy.
- If your BMI is between 18.5 and 24.9, you can gain up to 16 kg.
- With a BMI of 25-29.9, feel free to gain up to 11 kg.
- If your BMI is more than 30, then you can only gain up to 9 kg.
Gaining weight during pregnancy gradually
Try to resist the temptation to immediately “eat for two” - it is important to gain weight gradually. In fact, during the first trimester, your body does not need additional kilograms - it copes as is. And given that in the first months you may feel sick in the morning, gaining weight in this case will not be easy. But as your pregnancy progresses in the second and third trimester, you will need to gradually and smoothly gain weight.
Here's a rough breakdown of how many extra calories you should eat for healthy pregnancy weight gain by trimester:
- First trimester: no extra calories needed.
- Second trimester: About 340 additional calories per day.
- Third trimester: About 450 additional calories per day.
This amount is based on the recommended intake of 2,000 calories per day. Remember that these recommendations are approximate and may change depending on your BMI and other factors (for example, if you are expecting multiple babies).
If you are not hungry, there is no need to force yourself to eat more than you want. Listen to your body. Follow healthy eating guidelines, and if you're unsure, discuss your calorie intake with your doctor.
Don't diet during pregnancy, but don't forget to watch what you eat. Include plenty of nutritious and healthy foods in your diet. Double helpings of chocolate and ice cream are not what your baby needs.
If you are underweight or overweight, your healthcare provider can help you eat healthy foods to keep both you and your baby healthy throughout your pregnancy.
Possible problems
Pregnancy.
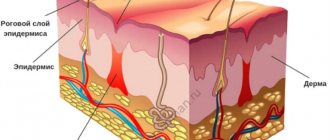
During pregnancy, favorable conditions are created for the development of fatty tissue, the biological meaning of which is to protect the unborn child. This is due to hormonal changes in a woman’s body, namely increased synthesis of progesterone and human chorionic gonadotropin (hormones that support pregnancy) and a deficiency of estradiol, produced by the ovaries mainly outside of pregnancy. The action of these hormones causes the deposition of adipose tissue mainly in the area of the mammary glands, buttocks, thighs, and abdomen.
In obese patients, pregnancy rarely proceeds without complications. The most common include gestational diabetes, or diabetes during pregnancy, arterial hypertension, hypercoagulation (increased blood clotting), cardiac dysfunction, toxicosis, preeclampsia (it is characterized by increased blood pressure, the appearance of edema, protein in the urine), urinary tract infections, miscarriage or post-term pregnancy. pregnancy (a condition in which pregnancy lasts more than 41-42 weeks), premature rupture of amniotic fluid, the birth of a child with a large body weight (more than 4000 g).
The most dangerous complication is preeclampsia - the most severe form of gestosis, the main symptoms of which are an increase in systolic pressure above 140 mmHg. Art., diastolic pressure above 80 mm Hg. Art., as well as proteinuria (loss of more than 3 g of protein per day in urine). In addition to the above symptoms, there may be signs of damage to other systems and organs: the appearance of headaches, abdominal pain, blurred vision. Laboratory tests reveal increased levels of liver enzymes and changes in the blood coagulation system.
Obesity also affects child development. As is known, folic acid plays a key role in the formation of the nervous system, and with obesity, its metabolism in the body of a pregnant woman changes, which can lead to the development of defects of the nervous system in the fetus.
Childbirth.
In obese women, not only pregnancy, but also childbirth itself occurs with a number of peculiarities, which is caused by hormonal changes. The internal system that triggers labor in such women remains imperfect by the end of pregnancy, and the lack of formation of a labor dominant (a focus of excitation in the brain) leads to post-term pregnancy, and subsequently to weakness of labor, the severity of which increases in proportion to the degree of obesity.
When labor is weak and cannot be corrected with medication, doctors are forced to resort to surgical delivery (caesarean section or forceps) to avoid acute oxygen deprivation in the newborn. But it is possible that the need for a cesarean section will be due to a discrepancy between the sizes of the pelvis of the mother and the fetus, since obese pregnant women, as mentioned above, are more likely to give birth to children with a large body weight.
In turn, surgical intervention is also associated with a large number of complications, since the severity of the subcutaneous fat layer impairs the healing of postoperative scars
You can purchase clever scales that analyze the mass of fat, muscles, and bones. During pregnancy, these scales can only be used for weighing, since they have not yet “learned” to take into account the weight of the fetus, placenta, and amniotic fluid.
In 6-30% of obese women in labor, bleeding occurs during childbirth, as well as in the postpartum period, the causes of which are both impaired contractility of the uterus and changes in the blood coagulation system.
It should also be remembered that obese women are at risk of developing carbohydrate metabolism disorders, that is, diabetes mellitus, therefore, 2 months after childbirth or after cessation of lactation, they need to be examined to determine blood glucose levels.