Biliary dyskinesia is an uncoordinated, untimely, insufficient or excessive contraction of the gallbladder, ducts, sphincters, which are functional in nature, causing a violation of bile secretion.
The outflow of bile and pancreatic secretions into the duodenum occurs due to the friendly work of the gallbladder, the cystic duct sphincter, the sphincter of Oddi, the work of which is coordinated by nervous influences and gastrointestinal hormones (cholecystokinin, secretin, etc.). If any of these regulatory mechanisms are disrupted, biliary dyskinesia may occur.
There are primary biliary dyskinesia as a manifestation of neurotic syndrome and secondary dyskinesia, which accompanies gallbladder diseases, including:
- chronic cholecystitis,
- violation of bile quality,
- cholelithiasis,
- cholangitis, etc.,
diseases of the duodenum and pancreas, as well as endocrine diseases, diseases of the kidneys, genital organs and other abdominal organs, connected by reflex and humoral connections, drug-induced dyskinesia of the biliary tract is possible (calcium preparations, contraceptives).
What is biliary dyskinesia (BID)?
JVP is a disorder of motor activity or motility of the gallbladder and bile ducts, which is accompanied by improper flow of bile into the duodenum and can manifest itself as pain in the right hypochondrium.
Bile is the most important participant in our digestion. It is produced in the liver, then enters the gallbladder, and from there it is delivered to the “place of work” - the duodenum. The gallbladder and ducts are the bile ducts. Their walls can contract and allow bile to move.
In some places, the muscle layer is thickened and forms sphincters - a kind of “gate” for bile. When food is not supplied and bile is not needed, the sphincters are closed. But already 10 minutes after the start of the meal, the secretion of bile begins. The gallbladder contracts and pushes it into the ducts. At the same time (precisely at the same time, and this is very important), the muscle “gates” open and bile quickly pours into the duodenum. It’s good if the bile ducts work smoothly. But “when there is no agreement among comrades”... This is dyskinesia.
What are the first symptoms that may indicate that you have dyskinesia?
It is not always possible to distinguish dyskinesia from other pathologies of the biliary system by clinical manifestations, but we will name the main symptoms. There are 2 main forms of ADHD with different clinical presentations.
Dyskinesia of the hypertensive type is characterized by periodically occurring paroxysmal pain in the right hypochondrium and the right half of the abdomen. Pain syndrome is a consequence of a sudden increase in pressure in the gallbladder, usually after errors in the diet (eating fatty, spicy, cold foods), or psycho-emotional stress. Pain occurs or intensifies 1 hour or more after eating. Many patients report pain in the heart area and palpitations. The pain may radiate to the right shoulder blade or shoulder. Dyskinesia of the hypotonic type is characterized by constant dull aching pain in the right hypochondrium without clear irradiation. Strong emotions and food intake increase pain and a feeling of fullness in the right hypochondrium. Patients often complain of decreased appetite, belching, nausea, bitterness in the mouth, bloating, and constipation.
There are intermediate variants of dyskinesia, when it is difficult to make a diagnosis based on symptoms alone, so if you more or less regularly experience discomfort in the right hypochondrium, you need to contact a gastroenterologist to find out what is really going on. Dyskinesia affects mainly women. A clear connection with the menstrual cycle is often noted (the occurrence of complaints or their greater severity during menstruation or, conversely, during menopause, as well as 1-4 days before menstruation). People of young age (20-40 years), asthenic constitution, low nutrition and even children are often affected.
General rules
Bile is constantly secreted by the liver and accumulates in the gallbladder between meals.
Its entry into the intestines after eating depends on the coordinated work of the entire organs of the biliary system: the hepatic ducts (right and left), the common hepatic duct, the gallbladder, the cystic duct and the common bile duct, which opens into the duodenum through the papilla of Vater (in the thickness of it There is the sphincter of Oddi, which regulates the flow of bile into the intestines). This sphincter, in turn, consists of three sphincters. The task of the sphincter apparatus is to regulate the flow of bile into the duodenum. Such a complex biliary pathway ensures the passage of bile and takes part in the formation of its composition, because the mucous membrane absorbs water, chlorides, bicarbonates, etc. A strong stimulator of bladder contraction is food intake. When it enters the duodenum, cholecystokinin , which regulates the contraction of the gallbladder. The time of its reduction depends on the composition of the food - rich and fatty foods cause a prolonged contraction until the stomach is emptied. When eating low-fat foods and in small quantities, the reduction is short-term. After contraction, the tone decreases and a period of bile filling begins.
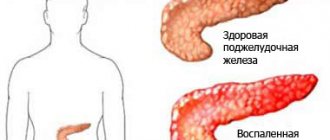
With biliary dyskinesia (BDSD), unsynchronous, excessive or insufficient contraction of the gallbladder, ducts and duct sphincters occurs. There are two types of disorders: hypertensive (with an increase in the tone of the bladder and sphincters and a sharp release of bile) and hypotonic (with a decrease in the tone of the sphincters and a sluggish outflow of bile from the bladder). These conditions are regulated by the autonomic nervous system and can be caused by nervous experiences, hormonal disorders, diseases of the gastrointestinal tract and nutritional disorders (constant consumption of fatty and spicy foods, excessive breaks between meals).
With hypotonic dyskinesia, stagnation of bile occurs in the gallbladder and insufficient flow into the digestive tract. Stagnation of bile can cause an inflammatory process in the gallbladder and be a prerequisite for the formation of stones, because the process of thickening of bile occurs in the bladder, and it becomes more saturated with cholesterol . A patient with this disorder is bothered by constant aching pain in the right hypochondrium, which can intensify or weaken. Nausea and vomiting, constipation , bitterness in the mouth, weakness and fatigue are also noted.
With the hypertensive type of dyskinesia, patients are bothered by acute paroxysmal pain in the right hypochondrium (during physical activity, running), periodic loose stools, nausea, vomiting with bile, and lack of appetite. Such patients are characterized by irritability, headache , increased fatigue, tachycardia , and sweating. Since dyskinesias are functional disorders, a balanced diet contributes to their correction.
The diet for biliary dyskinesia and liver diseases is based on the same principles, so the main table is Table No. 5 , with the introduction of different products taking into account the type of dyskinesia.
Basic principles of nutrition:
- The amount of refractory fats (lamb, pork, beef, goose, duck) is limited, which are difficult to digest and also increase fatty hepatosis. Butter is allowed from animal fats; it is better absorbed and is a source of retinol and arachidonic acid.
- The amount of protein corresponds to the physiological norm (100 g).
- Contains lipotropic products (cottage cheese, egg whites, fish, lean meat).
- Food is cooked in water (steam) and baked; frying is excluded.
- Food is crushed for hypertensive dyskinesia and grinding is not necessary for hypotonic dyskinesia.
- Fractional meals (up to 5-6 times).
- Salt is limited to 8 g.
- Liquid up to 1.5–2 l.
Calorie content must correspond to human energy expenditure. A diet with low energy value leads to fatty infiltration of the liver, cell death with the development of connective tissue.
Extractive substances (broths), cholesterol-containing products, spices, and whole milk are limited. Fast food, chips, salted nuts, sparkling water, smoked meats, and sausages are excluded.
In case of hypotonic dyskinesia of the biliary tract and after cholecystectomy in the presence of bile stagnation syndrome, it is necessary to stimulate the biliary system with choleretic products. For this disorder, a variation of Diet No. 5 - Table No. 5 L/F (lipotropic fat). Since in this pathology it is necessary to stimulate bile secretion, improve bile circulation and the motor function of the bladder and intestines, the diet contains a high content of fats, mainly vegetable, and fiber (vegetables, fruits, wheat bran), which have a choleretic effect.
, easily digestible carbohydrates (sugar, honey, sweets, preserves, jams, sweet pastries), which contribute to bile stagnation, are limited or excluded (in case of obesity In general, this is a complete diet with a physiological protein content, enriched with lipotropic substances that prevent fatty liver degeneration ( fatty hepatosis ).
For biliary dyskinesia in adults of the hypotonic type, the diet should include as many foods as possible with a choleretic effect:
- Vegetable oils should make up 50% of the total fat. They are involved in the synthesis of prostaglandins , which dilute bile and enhance contraction of the gallbladder. It is important to consume vegetable oils without heat treatment (for dressing salads, ready-made cereals and soups).
- Almost all vegetables, fruits and berries stimulate bile secretion and also relieve constipation . This point is important, since daily bowel movements have a tonic effect on the bile ducts. The most pronounced effect is found in oranges, avocados, tangerines, melons, watermelons, prunes, pears, lemons, and among vegetables - pumpkin, dill, rhubarb, spinach.
- Juices - cabbage, beetroot, lingonberry.
- Wheat bran (30 g per day). They are steamed with boiling water and, once swollen, added to all dishes, 2 tablespoons three times a day. Bran improves the flow of bile and reduces the likelihood of stone formation, since it reduces the cholesterol content in bile.
- Egg yolks.
- Frequent and small meals are important - this improves the flow of bile, and it is also advisable to expand physical activity.
For dyskinesia of the gallbladder of the hypertensive type, Diet No. 5 , but with a reduction in the total amount of fat to 60 g, a decrease in the amount of vegetable oils (up to exclusion) and fiber. Slightly increase the amount of simple carbohydrates. Diet No. 5Sh can also be considered as a nutrition option . It provides maximum sparing of the liver and other gastrointestinal organs and reduces the intensity of bile secretion. Characterized by a reduced amount of fat, with the exception of products containing cholesterol , extractives (broths) and coarse fiber (radish, radish, bran, garlic, mushrooms, cucumbers, onions, sweet peppers). In the diet of such patients, raw vegetables and fruits should be excluded - only baked or stewed ones can be consumed.
Meals include:
- soups, pureed vegetables, broths are excluded;
- lean meat and fish (preferably chopped);
- eggs are limited to one per day (whites only);
- milk, low-fat unleavened cottage cheese;
- baked and stewed vegetables (potatoes, zucchini, cauliflower, pumpkin, carrots);
- ripe, sweet fruits and berries in the form of compotes, mousses, jellies and pureed fruits;
- fruit and berry juices.
For all types of dyskinesia and symptoms of irritability and neurosis, an increased content of magnesium in the diet is indicated and a magnesium diet can be used. It reduces muscle spasm, reduces excitability and has an analgesic effect. The diet contains wholemeal bread, buckwheat and millet cereals, bran decoction, vegetables and fruits, dried fruits.
Intestinal dyskinesia (or spastic colitis ) is also a functional disorder that is manifested by pain, flatulence , changes in stool and abdominal discomfort. The motor function of the large intestine is most often impaired, and at the same time, spastic or atonic states are noted in its different parts, but no organic changes are detected. The main cause of intestinal dyskinesia is stress (chronic or acute) and symptoms of the disease may appear several weeks after it. In addition to gastroenterological complaints, the patient has neurotic disorders (anxiety, nervousness , worsening mood, depressive states , decreased performance). constipation occurs , less often it alternates with diarrhea .
Treatment depends on the form of intestinal dyskinesia: laxatives, motor stimulants, antispasmodics (for constipation) and absorbent, astringent, enveloping agents (for diarrhea) against the background of sedatives and tranquilizers. Relieving anxiety may require the participation of a psychologist.
Much attention is paid to nutrition and food intake.
- Small meals - it is important not to overeat and not overload the intestines.
- Boiled and baked dishes.
- Rye bread.
- Daily consumption of fermented milk products.
- Porridges cooked in water (any kind, exclude rice for constipation).
- Limit (exclude) baked goods, flour products, spices, smoked meats, fatty meats and fish, and spicy dishes.
- Quitting alcohol.
- Exclude turnips, radishes, radishes, garlic, mushrooms.
For constipation, the introduction of products that stimulate bowel movements is justified. Diet No. 3 may be effective in this case . This is a complete diet that you can stick to constantly. It includes foods that enhance intestinal motility (vegetables, fruits, baked goods with bran, cereals, fermented milk drinks, bran, prunes, fiber, beets, honey).
Products that increase fermentation and rotting (fried foods, legumes, simple carbohydrates, fatty foods) are excluded. On an empty stomach, it is recommended to drink water with honey, juices, and at night - kefir, infusions of dried fruits (prunes, dried apricots) and then eat steamed fruit or simply eat a portion of fresh fruit. It is necessary to exclude foods that delay bowel movements: chocolate, dogwood, jelly, cocoa, strong tea, lingonberries, black coffee, pomegranate, blueberries, pears, pasta, red wine, delicate cheeses.
Why does this disease occur?
The causes of the disease are dysfunction of the central nervous system, various diseases of internal organs, previous infections and helminthic infestations, dietary disorders, intoxication of the body and allergies. Many experts consider dyskinesia to be the beginning of gallstone disease.
Violation of the correct outflow of bile can lead to changes in its composition, which is one of the factors in the development of gallstone disease; stagnation in the gallbladder, characteristic of GIB, as well as reflux of intestinal contents into the biliary system, are fraught with the addition of inflammatory changes (cholecystitis). However, timely detection, treatment and prevention of VADP can prevent these complications.
Menu (Power Mode)
For dyskinesias, the diet must be followed constantly and, if followed correctly, various complications ( cholecystitis , cholangitis , cholelithiasis) can be prevented. The basis of nutrition for these disorders is Table No. 5 , to which adjustments are made for dyskinesia of the hypotonic type:
- In every meal, it is advisable to include vegetables and fruits (in any form), vegetable oils, alternating corn, sunflower, flaxseed, and olive.
- Be sure to include bran in all dishes in its natural form or after steaming it.
- It is better to eat whole grains and dried fruits daily.
- At night - fresh kefir.
- 150 g of bran bread and 100 g of rye bread.
Example menu for hypotonic dyskinesia
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Example menu for hypertensive dyskinesia
During the day, 200 g of wheat bread (white) and 30 g of sugar are allowed.
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
What examinations need to be carried out for ADHD?
Diagnostic tests for ADHD can be divided into 2 groups: screening and clarifying.
Screening methods:
- Transabdominal ultrasonography of the abdominal organs (ultrasound);
- Functional liver tests (determination of the level of ALT, AST, GGTP, alkaline phosphatase), pancreatic enzymes in the blood and urine;
- Esophagogastroduodenoscopy with targeted examination of the papilla of Vater.
The main method for diagnosing motility disorders of the biliary system is ultrasound. It allows you to identify violations of bile homogeneity, a “disabled” gallbladder (for differential diagnosis with cholelithiasis), in 80% of cases it provides information about the anatomical and topographic state of the gallbladder and in 45% - about the state of the large bile ducts. In a clinic setting, as a rule, the use of screening research methods is sufficient. At subsequent stages, various more complex clarifying methods can be used, for example:
- Ultrasound with assessment of the functional state of the gallbladder and sphincter ODDI;
- Endoscopic ultrasonography;
- Staged chromatic duodenal sounding, etc.
How is the treatment carried out?
Treatment is outpatient. Hospitalization is indicated only for severe concomitant pathology. Dieting plays a huge role in effective treatment, but not in the usual sense for weight loss, but in consuming high-quality recommended foods.
With hypertensive dyskinesia, limit the consumption of foods that cause contraction of the gallbladder: fatty, meat products, vegetable oil, products made from fatty dough, beer, carbonated drinks, ice cream.
For hypotonic dyskinesia, foods that stimulate contraction of the gallbladder are recommended: fruits, vegetables (carrots, cabbage, tomatoes), vegetable and animal fats (sour cream, cream), foods rich in magnesium salts, coarse plant fiber (bran, buckwheat, apples, rose hip decoction ).
Authorized Products
- Butter. Vegetable fats (olive, corn, flaxseed, sunflower) are included in case of hypotension of the gallbladder and the ratio with animals should be 1:1. Vegetable oils that have not undergone heat treatment cause the production of cholecystokinin , which stimulates the formation of bile. A prerequisite is that all oils are introduced into the finished dish in their natural form.
- Dried wheat bread. For hypotension - wheat bread with bran and rye. Only stale bread is allowed; biscuits, whole grain bread and bran bread are allowed. For the whole day: 150 g of wheat bread and 100 g of rye bread are allowed.
- Soups with vegetable broths (from cereals, vegetables or noodles). You can eat borscht and cabbage soup, beetroot soup, and fruit soups.
- Lean beef, rabbit, chicken, veal. You can boil them and make beef stroganoff from boiled meat; you can bake them after boiling. Chopped products (steamed or baked meatballs, cutlets, meatballs and dumplings) are preferable for bladder hypertonicity.
- Baked lean fish, fish stuffed with vegetables, steamed and baked fish cutlets, soufflés and quenelles.
- Cereal dishes include crumbly porridges made from rice, buckwheat and oatmeal, viscous semolina, and pasta.
- Fermented milk products should be chosen as low-fat. It is recommended to consume low-fat cottage cheese daily (in its natural form and as part of dishes). Milk and sour cream are added only to dishes.
- Eggs are allowed to be eaten as an omelet or soft-boiled. The number of eggs (up to one per day and without yolk) is limited in case of hypertension.
- Various boiled/stewed vegetables, vegetable caviar, carrot, pumpkin, green pea puree. For hypotension - vegetable salads with oil. Mainly the diet should contain cabbage of all varieties, beets and carrots, pumpkin, dill, parsley.
- Fruits and berries should be chosen non-acidic and consumed in the form of compotes, jelly, fruit drinks, infusions (fresh only for hypotension of the gallbladder).
- Sweets (marmalade, honey, jam, sugar 30 g per day are limited in case of hypotonicity of the gallbladder.
- Drinks: rosehip infusion, vegetable juices, weak tea (preferably with milk), bran decoction, still mineral water.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| eggplant | 1,2 | 0,1 | 4,5 | 24 |
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| broccoli | 3,0 | 0,4 | 5,2 | 28 |
| Brussels sprouts | 4,8 | 0,0 | 8,0 | 43 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| salad pepper | 1,3 | 0,0 | 5,3 | 27 |
| parsley | 3,7 | 0,4 | 7,6 | 47 |
| iceberg lettuce | 0,9 | 0,1 | 1,8 | 14 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
| dill | 2,5 | 0,5 | 6,3 | 38 |
Fruits | ||||
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Nuts and dried fruits | ||||
| raisin | 2,9 | 0,6 | 66,0 | 264 |
| dried figs | 3,1 | 0,8 | 57,9 | 257 |
| dried apricots | 5,2 | 0,3 | 51,0 | 215 |
| dried apricots | 5,0 | 0,4 | 50,6 | 213 |
| prunes | 2,3 | 0,7 | 57,5 | 231 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| oat groats | 12,3 | 6,1 | 59,5 | 342 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| rice | 6,7 | 0,7 | 78,9 | 344 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
| noodles | 12,0 | 3,7 | 60,1 | 322 |
| buckwheat noodles | 14,7 | 0,9 | 70,5 | 348 |
Bakery products | ||||
| bran bread | 7,5 | 1,3 | 45,2 | 227 |
| whole grain bread | 10,1 | 2,3 | 57,1 | 295 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jelly | 2,7 | 0,0 | 17,9 | 79 |
| marshmallows | 0,8 | 0,0 | 78,5 | 304 |
| milk candies | 2,7 | 4,3 | 82,3 | 364 |
| fondant candies | 2,2 | 4,6 | 83,6 | 369 |
| fruit and berry marmalade | 0,4 | 0,0 | 76,6 | 293 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
| Maria cookies | 8,7 | 8,8 | 70,9 | 400 |
Raw materials and seasonings | ||||
| honey | 0,8 | 0,0 | 81,5 | 329 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
Dairy | ||||
| kefir 1.5% | 3,3 | 1,5 | 3,6 | 41 |
| Ryazhenka | 2,8 | 4,0 | 4,2 | 67 |
Cheeses and cottage cheese | ||||
| cottage cheese | 17,2 | 5,0 | 1,8 | 121 |
| cottage cheese 1% | 16,3 | 1,0 | 1,3 | 79 |
Meat products | ||||
| beef | 18,9 | 19,4 | 0,0 | 187 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken breast | 29,8 | 1,8 | 0,5 | 137 |
| boiled chicken drumstick | 27,0 | 5,6 | 0,0 | 158 |
| boiled turkey fillet | 25,0 | 1,0 | — | 130 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Fish and seafood | ||||
| flounder | 16,5 | 1,8 | 0,0 | 83 |
| pollock | 15,9 | 0,9 | 0,0 | 72 |
| cod | 17,7 | 0,7 | — | 78 |
| hake | 16,6 | 2,2 | 0,0 | 86 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
| corn oil | 0,0 | 99,9 | 0,0 | 899 |
| linseed oil | 0,0 | 99,8 | 0,0 | 898 |
| olive oil | 0,0 | 99,8 | 0,0 | 898 |
| sunflower oil | 0,0 | 99,9 | 0,0 | 899 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| green tea | 0,0 | 0,0 | 0,0 | — |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| peach juice | 0,9 | 0,1 | 9,5 | 40 |
| plum juice | 0,8 | 0,0 | 9,6 | 39 |
| tomato juice | 1,1 | 0,2 | 3,8 | 21 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| rose hip juice | 0,1 | 0,0 | 17,6 | 70 |
| * data is per 100 g of product | ||||