Menopause is a physiological process associated with an increase in hormone deficiency of the hypothalamic-pituitary-ovarian axis. The pool of ovarian follicles capable of synthesizing female sex hormones is gradually depleted. In response to the sequence of endocrine changes that occur during perimenopause, perimenopause, and postmenopause, systemic somatic and emotional disorders appear. The skin is a target organ for sex hormones. In women, the trophism and appearance of the skin are most significantly influenced by female sex hormones: estrogen and progesterone. However, this review also highlights the effects of other hormones on the skin and subcutaneous fat.
During menopause, low estrogen concentrations are responsible for increased vascular permeability and decreased vascular tone, which lead to impaired microcirculation and are important factors predisposing to the development of cellulite. The effect of estrogen deficiency on the connective tissue of the skin includes a decrease in the production and local content of type I and III collagen and elastin, which also contributes to the development of cellulite.
This article presents the diagnostic methods and clinical types of cellulite, as well as the main instrumental and manual procedures used to treat cellulite. We looked at the use of drugs containing ingredients that help improve the metabolism of subcutaneous adipose tissue, increase blood and lymph circulation, and are used in cosmetology and aesthetic medicine. In addition, we provide a variety of opinions regarding the effectiveness of the treatments presented here.
Key words: menopause, cellulite, hormones, microcirculation, estrogen(s)
The period of menopause is, as a rule, a long process, accompanied by rapid hormonal changes, which are manifested by somatic systemic disorders and lability of the emotional sphere. The pool of graafian follicles responsible for the production of female sex hormones becomes depleted. Hormonal deficiency can lead to the development of numerous dermatoses and possibly increase existing manifestations. Frequently occurring skin defects are a consequence of these disorders, resulting in skin discoloration, hirsutism or cellulite. Properly selected therapy can improve the appearance of the skin and, therefore, improve the quality of life of women during menopause.
Definition of cellulite
The definition of cellulite was first voiced by French doctors in 1922 [1]. From a medical point of view, these are fibrous and edematous changes in the subcutaneous layer, lipodystrophy or edema, fibrous degeneration of connective tissue [2]. With this disease, degenerative changes in connective tissue occur due to impaired microcirculation. Cellulite is more often considered as a disease, as the WHO definition shows that it increasingly negatively affects the mental state of women and men [3].
Etiology of cellulite
The key cause of cellulite is considered to be hormonal imbalance, or more precisely, too high a concentration of estrogen compared to progesterone, that is, relative hyperestrogenism [4]. This hormonal situation can occur physiologically during pregnancy, puberty, menopause, as well as when taking systemic hormonal contraceptives or during hormone replacement therapy. The development of cellulite largely occurs under the influence of two processes that constantly occur in fat cells - lipogenesis and lipolysis.
In adipose tissue, consisting of adipocytes, fat synthesis and breakdown occurs. Lipogenesis supports the accretionary growth of adipose tissue, and lipolysis is a metabolic process that causes the breakdown of stored fat. Both of these processes are influenced by exogenous and endogenous factors. In the prevention of cellulite, it is important to maintain a balance between both processes. Local therapy is aimed at changing adipocyte metabolism and should limit lipogenesis and activate lipolysis.
Lipolysis is a process of destruction, disintegration and reduction of lipid accumulation in adipose tissue cells and muscles, occurring with the participation of lipase. Endogenous factors regulating lipolysis include hormones and neurotransmitters such as epinephrine and norepinephrine (has a weaker effect than adrenaline), estradiol and testosterone, adrenocorticotropic hormone (ACTH), growth hormone, thyrotropin (TSH, thyroid-stimulating hormone), leptin, antidiuretic hormone and glucagon. Epinephrine binds to receptors on the surface of β3 adipocytes, activates G protein, which excites adenylate cyclase, and ultimately increases the concentration of cyclic AMP (cAMP). Protein kinase, activated by cAMP, stimulates hormone-sensitive lipase, which causes the breakdown of accumulated lipids.
Neutral fat lipase (known as desnutrin) hydrolyzes triglycerides (TG) into diglycerides, and hormone-sensitive lipase degrades diglycerides into monoglycerides [5]. Glycerol and free fatty acids are the end products of lipolysis (free fatty acids) and serve as a source of energy for cells.
Cyclase inhibitory insulin is a hormone that blocks the process of lipolysis and stimulates the activity of lipoprotein lipase (LPL), responsible for lipid synthesis and the uptake of free fatty acids. The process of lipogenesis also depends on SREBP-1, a transcription factor whose expression is increased by insulin. For this reason, low concentrations of this hormone can support the process of lipolysis [6].
According to the adipocyte receptor theory, alpha receptors enhance lipogenesis, but beta receptors support lipolysis. Epinephrine, a catecholamine, comes mainly from the medullary layer of the adrenal glands and the fibers of the sympathetic nervous system, and stimulation of fat cells through alpha and beta adrenergic receptors is one of its functions. The consequence of its action is the influence on both types of receptors. The number of beta adrenergic receptors decreases under the influence of factors such as age, resulting in an increase in the amount of adipose tissue in response to the action of alpha receptors. This may be a reason for the accumulation of fatty tissue in menopausal women. This ratio causes a potential undesirable effect of anti-cellulite therapy [7].
Catecholamines, with the help of beta receptors, accelerate the metabolic process, while carbohydrates and fats are consumed sparingly [8]. A consequence of decreased estrogen levels during menopause is an imbalance between norepinephrine, dopamine, serotonin or endorphins. Increased secretion of neuroendocrine glands during menopause may be a result of stress. An increase in the secretion of norepinephrine indicates the absence of stable functioning of the autonomic nervous system. During this period, an increase in cortisol production is associated with menopause and at the same time with a high concentration of adrenaline and norepinephrine [9].
Basically, estrogens are the hormones responsible for the development of cellulite, since they are responsible for the organization of adipose tissue. In women, the production of adipose tissue does not depend on the amount of food eaten. The development of adipose tissue depends on the local influence of hormones. Aromatase, whose activity increases during menopause, affects the deficiency of ovarian estrogens [10], as well as the metabolism of lipids and glucose. This process leads to an increase in adipocytes, which, under the influence of pressure on blood and lymphatic vessels, causes an increase in local pressure, increases the load on the vessel wall, and also affects microcirculation. The lack of sex hormones during menopause has a negative effect on the vascular system [8]. It has been proven that there is a close relationship between venous circulation disorders and pathological changes in adipose tissue [3].
The PPAR group of nuclear receptors influences the metabolism of adipose tissue. These receptors are one of three types of PPAR gamma receptors that influence adipocyte maturation and diversification. They stimulate lipid accumulation and enhance adiponectin synthesis [6]. PPAR alpha receptors are type 2 receptors that influence beta-oxidation of free fatty acids and serve as regulators of lipogenesis [11]. Peroxisome proliferator-activated receptors PPAR influence the process of lipolysis through retinolic acid and conjugated linoleic acid (CLA) [2]. Estrogens activate the action of α-type adrenergic receptors and support the accumulation of adipose tissue in the thighs, hip joints and pelvis, and also affect the dilation and increase in the permeability of blood vessels. This leads to the appearance of microemboli and microedema. Estrogens interfere with the process of lipolysis and promote lipogenesis. They affect the increased amount of glycosaminoglycans (GAGs), which contribute to the deterioration of microcirculation (fluid accumulating in the intercellular space causes swelling, which causes microcirculation impairment).
Progesterone has a relaxing effect on smooth muscle fibers and can lead to venostasis, causing adverse morphological and functional changes [3]. Impaired microcirculation can cause a local increase in pressure and maintain increased venous permeability, which promotes slow blood flow and increases blood viscosity, leading to the formation of leukocyte traps. During certain periods of menopause, in addition to estrogen, the development of cellulite is influenced by other hormones, such as progesterone, growth hormone, melatonin, dehydroepiandrosterone, androgens or insulin, which may additionally lead to changes associated with improper transformation of fats and carbohydrates.
In premenopause, despite a decrease in the concentration of estradiol in the blood plasma and luteal insufficiency caused by more rare ovulations, a condition resembling hyperestrogenism may occur, and this creates conditions for the development of fatty cellulite along with a tendency to edema.
Another thing is a pronounced estrogen deficiency in postmenopause, since it supports the peripheral production of androgens, which can lead to the appearance of relative hyperandrogenism in older women [12], which can affect a change in the location of adipose tissue: a decrease in its content in places typical for women and development in the abdomen and torso, which leads to the appearance of the androidal (visceral) structure of the torso [13]. With age, due to decreased estrogen stimulation, the blood supply to the skin deteriorates, suppressing the function of fibroblasts, disrupting the normal synthesis of collagen fibers and reducing the number of elastic fibers. Under the skin, irregularities that are noticeable to the touch may appear - conglomerates in edematous connective tissue, emphasized by the lack of elasticity of the skin. Such changes are characteristic of cellulite.
Among the factors predisposing to the development of cellulite, in addition to the direct influence of hormonal disorders, it should be noted mainly genetic factors. There are familial tendencies towards improper deposition of adipose tissue and its characteristic organization with at the same time undeveloped muscle mass. Poor eating habits are other, non-hormonal risk factors for cellulite. Increased consumption of carbohydrates and fats maintains hyperinsulinemia, which, among other things, intensifies the process of lipogenesis and is one of the decisive etiological factors. A poorly balanced diet with a lot of preservatives and salt in food maintains fluid retention, which leads to edema. Other factors are low physical activity and a sedentary lifestyle, which disrupt normal microcirculation and support the accumulation of adipose tissue.
Nicotine and many other substances contained in cigarette smoke cause constriction of blood vessels, which leads to tissue hypoxia. After some time, weakening of blood vessels and improvement of oxidation conditions leads to the effect of reactive oxygen species on the process of hypoxia - reoxygenation.
Peripheral vasodilators, which are used in the treatment of arterial hypertension, can have an effect on the development of cellulite: beta blockers, antihistamines and exogenous estrogens [4].
Incorrectly chosen clothing and shoes, especially wearing tight-fitting clothing, definitely interferes with venous outflow. In addition, high-heeled shoes, through their negative impact on the lower leg muscles, interfere with good posture and weaken the function of the lower leg muscle pump when moving venous blood to the heart.
To prevent cellulite, it is very important to pay attention to all the factors predisposing to its formation. Some factors have a significant influence on the development of cellulite, such as genetic factors, and are beyond the range of any possible change, so it makes sense to focus on eliminating the factors that we can have a real influence on: changing an unsuitable diet or leading a more active lifestyle.
Flight or fight
The answer to the question of which hormone is responsible for cellulite would be incomplete if we did not mention adrenaline.
The human body has been formed over centuries. The hormonal system, which today many are strenuously trying to correct in order to eliminate some external manifestations that cause aesthetic discomfort, has been developed for the same amount of time.
Take, for example, the hormone adrenaline. Everyone knows that it is produced by the body in response to a stressful situation. Let's look at this point in more detail, and now you will understand why.
The substance is produced by the adrenal glands at those moments when a person needs to mobilize all his resources at lightning speed. This circumstance was very helpful for primitive people. Now we no longer need to fight mammoths or representatives of other communities, fight with someone or, on the contrary, run away. But the body still classifies many situations as a threat, in response to which hormones are produced.
However, instead of the principle of “fight or flight,” others have emerged in modern society: “be silent and smoke.”
When the reaction to a stressful situation is trembling of the body, limbs, increased breathing, dilation of the pupils, then the hormones released are unlikely to cause cellulite. In order to properly throw out the accumulated negativity, you need to transform the response into something useful for the body. Don't shake with anger, but shake in exercise machines or group Zumba classes.
https://youtu.be/dFsnmTvbxzw
Clinical signs of cellulite
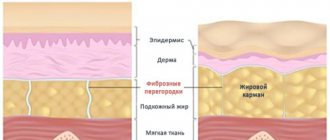
Clinical signs of cellulite are nodular, uneven formation of the skin surface. From a medical point of view, the structure of cellulite tissue differs from adipose tissue, first of all, by an increase in the number and hypertrophy of adipocytes and a violation of the proportion between saturated and unsaturated fatty acids included in these cells, unfortunately in favor of saturated fatty acids [7].
Regarding the characteristics of both sexes, differences associated with the structure of subcutaneous adipose tissue cause the appearance of lipodystrophy mainly in women, and in men exclusively in pathological conditions and when using antiandrogen therapy (for example, in the treatment of prostate cancer). Cellulite in men is localized in the neck and abdomen [7].
In women, cellulite often appears in the thighs, abdomen and buttocks, i.e. in places that have many receptors responsible for lipogenesis [2].
Until now, no one has been able to prove the connection between cellulite and obesity, since cellulite also appears in slender and active people.
There are three main clinical types of cellulite:
• adipose – excessive development of adipose tissue;
• lymphatic – transitional, intensively appearing mainly before menstruation;
• imaginary - appears due to weakened tension of the gluteal muscle, clearly visible on the back of the thighs; this condition can be improved by proper exercise [14].
Due to the nature of skin changes, cellulite can be divided into:
• hard type (in women involved in sports, when strong connections between neighboring cells in the skin and well-developed muscles are characteristic);
• thin form (in women of perimenopausal age, appears after dieting; muscle pliability, weakly stretched and loose skin are characteristic);
• edematous form (the most severe form, appears in women with severe diseases of the cardiovascular system) [2].
Myth
Cellulite is a sign of skin aging.
IS IT TRUE
Lipodystrophy can develop at any age, starting from adolescence, but more risk factors accumulate over the years:
- these are also bad habits,
- and lack of mobility,
- and a generally unhealthy lifestyle, leading to disturbances in blood supply and lymphatic drainage in fatty tissue.
By the way, the appearance of the first signs of cellulite in adolescence is more a norm than a pathology: such changes are directly related to the level of female hormones - estrogens. As a girl grows up, hormonal changes in the body occur, and at some point this can lead to the appearance of depressions and bumps on the skin.
Then they may well disappear on their own, but you still need to pay attention to their appearance, this is a sign of the body’s hereditary predisposition to lipodystrophy. Note that, according to various sources, 80–95% of women of the “European” race have such a predisposition, although to varying degrees, but black and Asian women are almost unfamiliar with cellulite.
Diagnosis of cellulite
The diagnosis of cellulite is established by a cosmetologist or dermatologist. The main method for diagnosing cellulite is a physical examination with palpation and visual assessment. There are many scales for assessing cellulite (Table I). The Nürnberger-Müller scale is the most commonly used. The DorisMaria Hexsel photonumeric scale for cellulite intensity, developed in 2009, is newer and considered more accurate (Table II). To assess this problem, based on photographs of 55 patients with cellulite, five key aspects were identified.
Table I.
Photonumeric cellulite intensification scale
| Clinical morphological signs of cellulite progression | Result |
| 1. Number of visible thickenings | 0 = no thickening 1 = small number; 1-4 visible thickenings 2 = average; 5-9 visible thickenings 3 = high number; over 10 noticeable thickenings |
| 2. Depth of thickenings | 0 – no changes 1 – superficial changes 2 – changes in average depth 3 – profound changes |
| 3. Various morphological patterns of superficial skin changes | 0 – no affected areas 1 – “orange peel” 2 – type of “pressed cottage cheese” 3 – “mattress” effect |
| 4. Degree of loosening and relaxation of the skin | 0 – no visible changes or folding of the skin 1 – slight folding 2 – medium folding 3 – excessive folding |
| 5. Nuremberger-Müller scale - in a standing position, “pinch” test (in the area of the relaxed gluteal muscle, the folds may not be visible, which makes it possible to differentiate the zero and first degrees) | 0 – zero degree 1 – first degree 2 – second degree 3 – third degree |
Table II.
The structure of the degree of cellulite intensity and its new typology
| Degree of cellulite intensity | New typology |
| 1-5 | Light form |
| 6-10 | Medium form |
| 11-15 | Advanced form |
The new classification scale mentions three stages of cellulite development:
The photonumeric cellulite change activation scale is extremely valuable in monitoring therapeutic anti-cellulite techniques and can be used to study affected patients [15].
In addition, cellulite can be assessed using specific tests: thermography (measures body surface temperature and color indicates tissue temperature), macrography, TEWL (transcutaneous dehydration measurement), device to measure skin lubrication or elasticity, video capillaroscopy (test evaluates the condition capillary filling: in the area of widespread cellulite, the tissue is poorly supplied with blood), electrical bioimpedance (determines the content of adipose tissue and water in the body). Computed tomography, magnetic resonance imaging and ultrasound are very effective in diagnosing cellulite.
But neither computed axial tomography nor magnetic resonance imaging can be used universally due to their high cost, and in the case of computed axial tomography, the radiation exposure of X-rays. Thus, ultrasound is a more general and objective method than the palpation scale. Cellulite assessment studies are performed using classic ultrasound scanners and high frequencies.
Classical ultrasound examination evaluates parameters such as the thickness of the dermis and subcutaneous fat layer, the echogenicity of both structures, as well as the boundary between the dermis and subcutaneous layer [16]. With a high frequency of ultrasound examination, the following parameters can be assessed: the thickness of the cuticle and dermis, the presence of edema, the echogenicity of the dermis and, most importantly, the process of formation of dermal papillae in the subcutaneous fat layer [17].