Diet for PCOS
Polycystic ovary syndrome, or PCOS, is a disease that occurs in women and is associated with the formation of a large number of cysts in the ovarian area. Most often this disease is caused by problems such as:
- overweight, obesity;
- insulin resistance;
- imbalance in the hormonal system, which can be caused by various factors.
Any woman can experience PCOS and if action is not taken in time, this disease can lead to infertility and other health problems.
Today it is known that adipose tissue, along with the ovaries, is the place where extragonadal synthesis of sex hormones from androgens occurs. That’s why it’s so important not to be overweight, because this causes an imbalance in the hormonal system due to the fact that some hormones are produced more and others less.
Diet for polycystic ovary syndrome becomes a priority, since very often after weight normalization there is an improvement in the picture of the disease.
When metabolic processes in the body are restored by reducing the amount of excess weight, the body itself begins to fight PCOS and, accordingly, its symptoms.
Excess weight is only a risk factor; polycystic ovary syndrome can also occur in women with normal weight, but this does not mean that metabolic processes and the functioning of the endocrine system are not disrupted, so such patients are also prescribed a diet. Such a diet will not be aimed at losing weight, but at normalizing metabolic processes and eliminating deficiency conditions.
Basic principles of losing weight with PCOS
There is an opinion that when diagnosed with PCOS it is impossible to lose weight and a vicious circle results: in order to eliminate this condition it is necessary to lose weight, but it is impossible to lose weight. This statement is completely wrong.
Losing weight with this disease is possible, but it should be gradual so as not to cause stress to the body and with a well-designed diet to meet all the body’s needs.
The diet is prepared individually for each patient, based on the results of diagnostic studies, the patient’s medical history, symptoms and course of the disease.
The basic principles of nutrition for PCOS are:
- monitoring the glycemic index (GI) of foods. Foods with a high GI provoke a large release of insulin into the blood and due to subsequent reactions, insulin resistance may develop, which is a provoking factor for polycystic ovary syndrome. Most high-GI foods are high in carbohydrates, and controlling the GI can mimic a low-carb diet. However, it is not advisable to give up carbohydrates; it is necessary to maintain a balance of fats, proteins and carbohydrates in the body so that all metabolic processes occur in accordance with the norm;
- reducing the amount of animal fats entering the body. Excess animal fats in the body provokes an increase in cholesterol in the blood, which can clog blood vessels and impede blood flow through them, due to which nutrients and oxygen will not reach the organs in the required quantities, thereby disrupting metabolic processes in the body;
- attention is paid to the work of the intestines, and for its functioning and preservation of the intestinal microflora, which plays a large role in metabolic processes, it is necessary to consume a sufficient amount of fiber, which is contained in plant foods;
- adhere to the principles of fractional nutrition, avoid strong feelings of hunger.
In addition to nutrition, it is necessary to engage in physical activity, because it has a beneficial effect on the body and organism. Also, during physical activity, hormones are released that improve mood and increase overall tone. You can go swimming, jogging or long walks in the fresh air, fitness or home workouts; in general, all types of moderate physical activity are welcome.
Polycystic ovary syndrome: answers to frequently asked questions
Special thanks to the user of the Supermomki wanna-kid forum for a well-written list of questions, which I answered. The list of answers is not finite. Write and ask. I'll add some more useful information. A list of abbreviations that doctors often use in their work in order to completely confuse everyone. And increase your importance (non-doctors often do this too - PCOS is the same as PCOS - polycystic ovary syndrome, the same as polycystic. - Multicystic ovary - the same as polycystic - more than 12 follicles in each ovary - Hyperandrogenism is the same as hyperandrogenism - an excess of one or more of the following hormones: testosterone, androstenedione, 17-hydroxyprogesterone, DHEA. These hormones are often mistakenly called androgens - male hormones. Erroneously, because they are normally present in both sexes . Men have a little more. Question 1. Regarding hormonal drugs - how long before planning a pregnancy with polycystic disease should they be stopped? A lot has been written about the dangers of hormonal drugs for the fetus. Personally, in the first month after the withdrawal, my periods come on their own, and then they no longer. That is, I can’t cancel it. What should I do in this case? Are hormones really so harmful? Will the gynecologist prescribe stimulation or will I have to take duphaston, in my case, if I don’t have my period even in the second month? This moment is unclear.
The list of answers is not finite. Write and ask. I'll add some more useful information. A list of abbreviations that doctors often use in their work in order to completely confuse everyone. And increase your importance (non-doctors often do this too - PCOS is the same as PCOS - polycystic ovary syndrome, the same as polycystic. - Multicystic ovary - the same as polycystic - more than 12 follicles in each ovary - Hyperandrogenism is the same as hyperandrogenism - an excess of one or more of the following hormones: testosterone, androstenedione, 17-hydroxyprogesterone, DHEA. These hormones are often mistakenly called androgens - male hormones. Erroneously, because they are normally present in both sexes . Men have a little more. Question 1. Regarding hormonal drugs - how long before planning a pregnancy with polycystic disease should they be stopped? A lot has been written about the dangers of hormonal drugs for the fetus. Personally, in the first month after the withdrawal, my periods come on their own, and then they no longer. That is, I can’t cancel it. What should I do in this case? Are hormones really so harmful? Will the gynecologist prescribe stimulation or will I have to take duphaston, in my case, if I don’t have my period even in the second month? This moment is unclear.
Hormonal medications used before pregnancy are not harmful.
At all. Indeed, many women have such irregular cycles that they cannot stop taking the medications. Here you need to keep the following in mind: Hormones containing antiandrogenic components may be unsafe for a male fetus. Anti - against, andros - man. The drugs Diane-35, Yarina, Jess have a pronounced antiandrogenic effect. As a matter of fact, this is what they were created for: excess body hair growth is optimally treated with these medications. But! It is better not to use them in the cycle before a planned pregnancy. Frankly speaking, their harmful effects on the fetus have not been proven. No pregnant woman in her right mind would allow experiments on her unborn baby. The opposite has not been proven either. Therefore, it is better to abstain. And if your doctor prescribed you a hormone before conception, it wouldn’t hurt to inquire about whether it has an antiandrogenic (remember the term!) effect. And most importantly: if the pregnancy test is positive, take any medications, especially hormones, only with the knowledge of your doctor! Question 2. Is it worth monitoring hormones? Doctors say differently and it is impossible to understand where money is being pumped out and where the truth is.
After all, if a diagnosis has already been made once, why recheck it? There is no need to monitor hormones. PKY either exists or it doesn’t. In some cases, I do not prescribe blood tests for hormones at all. The fact is that international standards for establishing this diagnosis do not clearly require hormonal confirmation. Excess of male hormones (hyperandrogenism) can be detected clinically (examination reveals excess hair growth, acne, oily skin) or laboratory. That is, if there are clinical signs of hyperandrogenism, laboratory confirmation is not required. And vice versa. The other side of the coin: I often strive to cancel the diagnosis of “polycystic ovary syndrome” already made by someone before me. To do this, I sometimes need to repeat hormone studies. Which, in turn, can be regarded by you as “pumping out money.”
PKY either exists or it doesn’t. In some cases, I do not prescribe blood tests for hormones at all. The fact is that international standards for establishing this diagnosis do not clearly require hormonal confirmation. Excess of male hormones (hyperandrogenism) can be detected clinically (examination reveals excess hair growth, acne, oily skin) or laboratory. That is, if there are clinical signs of hyperandrogenism, laboratory confirmation is not required. And vice versa. The other side of the coin: I often strive to cancel the diagnosis of “polycystic ovary syndrome” already made by someone before me. To do this, I sometimes need to repeat hormone studies. Which, in turn, can be regarded by you as “pumping out money.”
Question 3. The question is not mine personally, but also a painful one - who makes the diagnosis: an ultrasound specialist, an endocrinologist or a gynecologist for hormones, or what? Often ultrasounds and hormones argue and women don’t know who to believe (a real case from a friend on the forum)
The diagnosis is always made by a clinician.
That is, not an ultrasound doctor, and not a laboratory assistant, and not a surgeon during laparoscopy. The diagnosis is made by a doctor sitting in an office, pen in hand, assessing all the available clinical information. And hormones, and ultrasound, and histology and, of course, examination with your own hands and eyes. In 2003, a conference was held in the glorious city of Rotterdam, at which reproductive specialists from all over the world met (well, almost all of them, the American and European associations), and established international standards according to which the same diagnoses should be made all over the world in the same situations. These standards are called the “Rotterdam criteria”. They are not a secret. Here they are: The diagnosis of PCOS is established in the presence of at least two of the three following symptoms: 1. menstrual irregularities and rare ovulation (eight or fewer menstruation per year) 2. clinical or laboratory hyperandrogenism. 3. multicystic ovaries, according to ultrasound examination. As you can see, ultrasound confirmation in itself, without other symptoms, does not mean anything. And vice versa. Ultrasound confirmation is not required. Thus, we cross off the ultrasound doctor from the list of doctors making diagnoses. The surgeon, by analogy, too. For hormones, no diagnosis is made, see the answer to the previous question. So what happens that ultrasound is not informative in any case? That is, you don’t need to look at him at all? Or is it informative, but only in conjunction with other studies? The second assumption is correct. That is, in addition to the very fact of polycystic (multicystic) ultrasound, there should be an ovulation disorder or hyperandrogenism. And if there is both ovulation disorder and hyperandrogenism, then ultrasound does not matter. All of the above does not mean that ultrasound is not necessary at all. Necessary. An experienced doctor can take a lot of information from an ultrasound examination. But the diagnosis of PCOS is still not made in the doctor’s office by ultrasound. Question 4. If you have such a diagnosis, how long does your clinic give you to get pregnant on your own?
After how many months would you recommend contacting a fertility doctor instead of a gynecologist? If you want to conceive and are unable to conceive, contact a fertility specialist. In all other cases - see a gynecologist. The point is not what your diagnosis is - you may not know all your problems and make the wrong decision, so the point is how long you have been sexually active and how regularly. WHO experts assume that there are problems if you have been sexually active for 12 months at least twice a week, also at least, and still have not become pregnant. I'm closer to 24 months. More women become pregnant in two years than in 12 months - verified. But, if you are over 35 years old, or have a lot of problems with gynecological health (don’t forget your husband), welcome to us after six months! To a reproductive specialist, of course. And a gynecologist will help you maintain your health for many years! More information about when to consider yourself infertile or infertile is in the article of the same name on our website. Read it slowly!
Question 5. A question that worries many polycystic women: personally, I was quite swollen due to hormones, now it’s very difficult to get in shape - the belly was, is and will be. When stopping hormonal medications, is it possible to return to my normal weight or is this a symptom that is “always with me”? sport goes without saying, but when I play sports, I personally lose everything except the “life preserver.”
Taking oral contraceptives does not increase the content of steroid hormones in a woman’s body, but, on the contrary, reduces it!
The exception is the first 1-2 cycles, when the hormones of the tablets are layered on top of their hormones, thus adding up and causing side effects. The typical, most common side effect is headache. But not obesity! “Lifebuoy” - excess weight is distributed in the abdominal area. Endocrinologists have a beautiful description of obesity - apple-type, characteristic of excess androgens, and pear-type - excess fat is deposited in the hips - characteristic of excess estrogen, which is considered more or less normal for a woman. What do you consider normal? It is possible that your ideal of female beauty is based on the vicious fashion instilled by models in the “coat hanger” style. The practice of cult of models weighing 40 kg (at best) is condemned, but not prohibited from showing. If this is not the case, read on. An excess of steroid hormones or insulin causes “gluttony” - an increase in the need for the amount of food and its severity. No one with PCOS wants to eat apples. But chocolate, kebabs and nuts - just like that! Increased calorie consumption in the absence of output (mobility does not increase proportionally) leads to hyperplasia of fat cells - an increase in their absolute number. Not only the specific gravity of fat in each cell, but precisely their number. Therefore, losing weight to your old weight is very difficult, sometimes impossible. It all depends on the scale of the changes. In such cases, you have to make Herculean efforts in the gym, with mediocre success. And don’t forget that we were talking about a hormonal disease - polycystic disease, and not about the cult of food in a single family. Thus, it is better to keep your weight under control and not allow it to gain. Don't lose weight before the beach season. And in most cases, hormonal pills have nothing to do with it at all. Question 6. How often should I be tested for predisposition to diabetes, check my sugar, etc.?
Is there a certain age when you should start worrying about this? The answer depends on whether you have a family history of diabetes. If so, and you also have PCOS, then pay attention! A glucose tolerance test with insulin should be done at least every five years! And save the research results so that they can be assessed over time. The emergence of clinically grown diabetes mellitus is a matter of time. Very often, women are confident that there is no diabetes in their family, boldly considering unclear results as negative. Grandfather died early, no one knows why. I don't know my dad. Etc. An unclear result when compiling a family tree cannot be considered negative. Often there is also an opinion that diabetes in a mother or grandmother arose due to stress, or was severely suffered by us due to the flu, injury, or something else. Diabetes mellitus is genetically determined. His appearance is predetermined. And the flu could be a reason to do a blood sugar test. We should not forget that the quality of medicine is improving. Mass screening of older people has not always been the case.
Question 7. Is it possible to somehow improve the condition of the ovaries besides hormones? After all, in fact, PCOS develops with increased sensitivity to insulin or increased production of certain hormones? I was once prescribed Siofor for 3 months, but the doctor has not made such prescriptions for a long time, relying only on COCs. I would like to know if there is still a chance to do without them.
Hormones do not improve the condition of the ovary.
They improve the condition of the endometrium. Impaired ovulation, the main symptom of PCOS, leads to disruption of the corpus luteum. And to increase the level of estrogen in the blood. Estrogens are hormones that are very necessary for a woman, they, in fact, make a woman feminine, but in the absence of progesterone, the main hormone of the corpus luteum, estrogens cause a precancerous condition of the endometrium. Today is pre-cancer. And tomorrow? PCOS is clearly associated with an increased incidence of endometrial cancer. Oral contraceptives, every single one, contain a progesterone analogue (we call it progestogen). Taking oral tablets for PCOS protects a woman from endometrial cancer. And a little bit for ovarian cancer. And there is another pleasant side effect - your period comes when it’s supposed to. Regularly. And not during a vacation at sea. And not when your beloved young man arrives. Conclusion: no one forces you to take oral contraceptives. But then your life will illuminate the history of your native city with a bright, but not very long-lasting flash... However, not everything is so bad. The shortening of life expectancy and quality of life in a woman with PCOS who does not take contraceptives is not double or even multiple at all. We are talking about several years of life, and even then on average for the population. It’s just that in the twenty-first century, science has accumulated enough data to claim that in case of PCOS, taking oral contraceptives brings more benefit than harm. Now you can answer your own question: is there a chance to do without them? And I move on to the next question, not asked, but obligatory for discussion: why is it necessary to treat polycystic ovary syndrome at all and what can be considered a satisfactory result of treatment? The answers will be surprisingly simple: If PCOS is associated with reduced fertility, then the goal of treatment is to get the woman pregnant quickly and, if possible, inexpensively. The true goal, however, is not pregnancy, but a child. Healthy child. Born not after a multiple or complicated pregnancy. And if we are not talking about conception, then the goal of treatment is to preserve the woman’s health, not only and not so much gynecological, but also general. Question 8. Another question about everyone’s favorite clostilbegite, which is prescribed for several cycles in a row in everyone’s favorite “certain” clinics: tell us about its benefits and its harms, opinions on this matter vary greatly.
Klostilbegit. It's clomiphene. Aka clomiphene citrate. The first effective drug to stimulate ovulation. For about forty years it was the only more or less working drug. Until gonadotropins were invented. Thanks to clostilbegit, many children were born. Therefore, clostilbegit is an honored veteran of reproductive medicine. And it’s too early for him to go to the dump! The fact is that clostilbegit is much cheaper than its gonadotropin competitors. And there is no hyperstimulation on it. In my practice there was none. The positives end there. Clostilbegit not only stimulates ovulation. At the same time, it spoils the endometrium, reducing the likelihood of embryo implantation. Therefore, there are fewer pregnancies. But they are cheaper and safer. Several years ago, it was believed that taking clostilbegite six or more times in a lifetime increased the likelihood of ovarian cancer. It has now been proven that ovarian cancer is associated not with clostilbegitis, but with polycystic ovary syndrome itself. Let me explain. Once in the USA, a scientific study was conducted to identify what factors reduce the life expectancy of Americans in order to eliminate these very factors. An interesting thing turned out: those Americans who had two or more lighters in their house lived significantly less! On this basis, it was even seriously proposed to introduce a tax on gas lighters. Of course, it was not lighters, but smoking that was the main factor influencing life expectancy. Lighters were a “cofactor” - a kind of information noise that made it difficult to make the right decision. Clostilbegit is a classical cofactor. And the real problem is PCOS. In order to restore the reputation of clostilbegite, it was necessary to conduct complex scientific studies - the so-called “double-blind study”. Read more about this here https://esquire.ru/ideas/richard-dawkins and https://ru.wikipedia.org/wiki/Double_blind_method Now it has been definitely proven that clostilbegit is a safe drug. But the reputation deteriorates quickly. Improves slowly. Currently, clostilbegit is the first drug used to stimulate ovulation in PCOS. Unless, of course, we are talking about IVF. And we usually don’t offer more than six attempts, because the increase in pregnancies after six attempts is very small. In this case, IVF gives more pregnancies per ruble spent than any alternative method.
Question 9. Can this disease be considered hereditary? How can it be prevented or predicted? Some sources write that even severe stress during puberty can be the cause, is this true?
No that's not true. Severe stress often causes ovulation disorders - nature took care of the woman - it is better to get pregnant when everything around is calm and good. The hypothalamus stops stimulating ovulation. And this condition has nothing to do with polycystic disease. However, on ultrasound, the ovary looks polycystic the same, regardless of the cause of ovulation disorders. Perhaps this was the reason for the emergence of the myth about the involvement of stress in the development of polycystic disease. But there is heredity, obvious. Moreover, the failure of multiple genes can lead to the same syndrome - polycystic ovaries. Geneticists call such diseases multifactorial - many causes, many factors, it is difficult to laboratory prove a cause-and-effect relationship.
For those who want to learn more about the genes of PCOS (as well as about any genetic diseases), there is the website omim.org. We launch PCOS (the English analogue of PCOS) in the search bar and count how many genes the site finds. Will find a lot. If you spend more time on the site, it’s easy to come to the conclusion that all known human diseases are transmitted only by inheritance, with the possible exception of gonorrhea and syphilis. Every joke has a grain of humor.
Will find a lot. If you spend more time on the site, it’s easy to come to the conclusion that all known human diseases are transmitted only by inheritance, with the possible exception of gonorrhea and syphilis. Every joke has a grain of humor.
Conclusion: PCOS is a genetically determined disease, but we cannot yet prove this in the laboratory. Question 10. Is hormonal therapy prescribed during pregnancy or is this in itself considered recovery?
Unfortunately, pregnancy cannot be considered a cure.
We can talk about winning in the first round. Hormonal problems are not going away. They just get a new status. PKYA remained as it was. Hormone consumption during pregnancy: All oral contraceptives are contraindicated during pregnancy. Absolutely. Metformin (aka Siofor, Metfogamma, Glucophage) - harm during pregnancy has not been proven. There are reports that drugs in this group have been successfully used during PCOS pregnancy, without harm to the fetus, and that this did not cause any problems in the child born after this. But the sample was small and there was no convincing evidence. Cunning Europeans are waiting for such studies to be carried out in third world countries and, probably, metformin will be approved for use during pregnancy. In the meantime, it's a set. And lastly: the use of progesterone drugs (Utrozhestan, Krainon, progesterone itself) may not be as useful as previously thought. Progesterone is the precursor of all androgens, and an overdose of it in PCOS can do more harm than good. Discuss these questions with your healthcare provider. To conclude the question: PCOS clearly worsens pregnancy outcomes. And we do not have effective drugs for this. Therefore, all preparation, both hormonal and non-hormonal, occurs before conception. I very often take time without making a woman pregnant until she is maximally prepared for pregnancy. Especially if you have PCOS. Especially if you are overweight. Question 11. What BMI is considered the “point of no return” for PCOS?
In what condition should you give up and admit your inability to have children? Under no circumstances.
In principle, the question is incorrectly posed. A normal BMI (body mass index) is up to 25. We consider thirty and above to be obese. But we must understand that these norms are artificial. That is, they were created on purpose to facilitate communication between doctors. For example, I’m coming to America: what are your results after IVF for PCOS with a BMI of 30? Such and such. I compare it with mine - it seems similar. I'm calming down. Let's move on to the next question. And so on all the time. Standards in medicine were invented so that doctors of related specialties could compare the results of their work in typical cases. What does this mean to you? The closer your BMI is to 25, the better - you will get pregnant faster and carry a pregnancy to term. Question 12. I quote the test tube: “Even singleton pregnancies with polycystic disease are associated with an increased risk to the health of both the mother and the fetus.”
What risks are they referring to here? Risks of miscarriage and premature birth.
Excess steroid hormones increase the likelihood of miscarriage. Excess weight increases this effect. The risk of gestosis, abnormal birth, and bleeding after childbirth increases slightly. Premature birth also does not add health to the fetus. Here we need to dwell in more detail on the concept of risk. Risk is not catastrophe. This is simply an increase in the chances of getting any problems. Let's say your age group has a 15% chance of miscarriage. Polycystic disease increases it by one and a half times (the figure is inaccurate, as it depends on other factors). Fifteen percent became twenty-two. One in five women will end up having a miscarriage. So now, shouldn’t we give birth? But four out of five women will give birth to healthy babies! The practice is much more difficult. Many factors are mixed there - tubal, inflammation, smoking, age - a lot of things. Often we cannot even accurately and quantitatively determine the risks. But you still have to give birth. The one who walks will master the road. You just need to know in advance. Ask your doctor what risks there are for me and my child when prescribing (or, conversely, not prescribing) this treatment? This is a good question, don't be shy to ask. Question 13. And another personal request - maybe it’s possible to put a diet for PCOS on your website?
The doctor printed this out for me, but I lost it, otherwise there would always be a hint. In general, if there are similar diets for the treatment of infertility and other diseases, it would be useful to always have them on hand. Recommendations for women with PCOS are constantly being optimized; the diet may be changed.
Write a letter to the ART nurses, we will send you the current version. Conclusion on the topic of PCOS: Women are different. Tall. And not really. With a large bust and with a small one. With a bad character and pleasant to talk to in any situation. With high insulin levels and not so much. With a large amount of androgens in the blood and with a low one. And everyone wants to love and be loved. And everyone wants to have children. As many children as you want. Then, when you want. And we, doctors, have the necessary knowledge and skills to help with this. We often snatch a woman from the crowd, declaring her unhealthy, in connection with current scientific ideas about what a healthy woman should look like today. And women get pregnant. They give birth. And we doctors periodically change our vision. And we instill it in women. Often replacing true goals with surrogate ones. My dear women! Don't worry about hormone levels! Don't count the follicles in the ovary! Talk to doctors in a language you understand! Demand it! And discuss the main questions: can I get pregnant and carry a child? With what probability and for how long? What are the risks for me and my child? What else do I need to know? And please read, read popular medical literature. She will help you ask the right questions. Good luck everyone!
Diet for polycystic ovary syndrome
Let's talk a little about the so-called “prohibited” and “allowed” foods during the treatment of PCOS. It is worth understanding that what enters our body directly affects our well-being and emerging diseases.
Generally speaking, the following products should be present in the diet:
- lean meat (beef, turkey, chicken);
- fish rich in protein and omega 3 polyunsaturated fatty acids (salmon, trout, salmon, pollock, hake, cod, etc.);
- chicken or quail eggs;
- vegetables and greens (it is better to eat at every meal for better absorption in the intestines);
- mushrooms;
- eat whole grain cereals or green buckwheat;
- give preference to flour products made from wholemeal rye flour;
- consume fats in the form of olive oil or avocado;
- olives and olives;
- introduce nuts and seeds into your diet (note that almost all nuts must be soaked before consumption);
- various types of berries;
- fruits with a little sugar;
- dairy products without sugar or with a minimal amount of it;
- herbal teas (before drinking tea from any herb, it is better to learn about its properties or consult a doctor; ginger tea usually has no contraindications and is beneficial for everyone);
- the use of spices that tend to relieve inflammation (turmeric, oregano, cumin).
Foods you should avoid in your diet:
- fatty meats;
- foods high in fat (margarine, heavy cream, etc.);
- processed foods (sausages);
- semi-finished products;
- milk chocolate and flour products;
- coffee and strong teas;
- foods high in starch.
All of the categories of foods described above are not part of a special diet for PCOS; sticking to eating “allowed” foods and avoiding “forbidden” ones should be part of the daily diet of all healthy people.
Several examples of menus for every day for a diet for polycystic ovary syndrome are displayed in the table.
| Menu No. 1 | |
| Breakfast | Low-fat cottage cheese with the addition of nuts or fruits. |
| Lunch | Crispbread and fruits (banana, apple) |
| Dinner | Fish, baked, oven-baked or steamed with vegetables. You can have juice without added sugar. |
| Snack | Vegetable salad with egg. |
| Not a late dinner | Cutlets or steamed meat. |
| Snack | Low-fat fermented milk product (kefir, yogurt). |
| Menu No. 2 | |
| Breakfast | Oatmeal or millet porridge with a small amount of butter or fruit. |
| Lunch | Avocado toast with egg. |
| Dinner | Vegetable soup. Garnish of green buckwheat and boiled chicken breast. |
| Snack | Lenten cookies. |
| Not a late dinner | Stewed cabbage with vegetables. |
| Snack | Homemade jelly. |
The menu for every day when dieting due to PCOS should be compiled based on your preferences and individual ratio of KBJU.
Areas of distribution of fat deposits
In addition to body mass index, the areas in which fat deposits are located are also important. The following types are distinguished:
- Abdominal (android). Fat is most often found in the abdominal area. This type is the most dangerous, since fatty tissue accumulates around organs, which leads to initial destabilization of blood pressure and diabetes mellitus. The risks of pathologies of the cardiovascular system increase significantly. Separately, there is lower abdominal obesity, in which fat accumulates in the buttocks and thighs. In this case, the effect on the spinal discs and large joints increases.
- Intermediate (mixed). In this case, fat deposits are evenly distributed throughout the body.
Causes of obesity
Pathology has various causes. Most often, the following factors can provoke this condition:
- drinking sweet carbonated drinks;
- low physical activity;
- the predominance of sugar in the diet;
- a number of genetic abnormalities;
- decreased metabolism;
- chronic lack of sleep;
- severe stress;
- the presence of hypothyroidism and other abnormalities of the thyroid gland;
- taking certain psychotropic medications;
- consuming carbohydrate foods in excess of the norm;
- eating disorders.
Obesity in women
If a patient is suspected of infertility, a series of tests and diagnostic procedures are prescribed to identify the health status. If a woman has a high BMI, an examination is necessary to determine the causes of excess weight.
Excess body weight in most cases negatively affects the ability to conceive. If pregnancy occurs, obesity can trigger the risk of premature termination and a number of complications in the development of the fetus.
Infertility due to obesity is most often caused by a lack of ovulation. Excess weight almost always leads to menstrual irregularities, which leads to problems with egg maturation. As a result, natural conception of a child becomes impossible.
Another reason for infertility in obesity is hormonal changes in the body. Most often, an overweight patient has hormonal imbalances, which leads to a number of serious complications for the entire body.
Obesity in a woman can cause the following complications:
- Development of polycystic ovary syndrome. The presence of such a syndrome leads to the appearance of endocrine infertility.
- Improper production of thyroid hormones. In this case, excess body weight is caused by hypothyroidism, which ultimately leads to decreased fertility.
- Diabetes. When type 2 diabetes mellitus appears in a woman’s body, serious disturbances in carbohydrate metabolism occur.
Infertility treatment in this case consists of eliminating excess weight. Most often, hormonal or other drug therapy is necessary.
Diet for PCOS for weight loss
A diet for weight loss should be based on the daily calorie consumption and activity of the patient. It is necessary to monitor the balance of proteins, fats and carbohydrates so that the skin, hair and internal condition remain normal. In everything, moderation and a varied diet are necessary for successful weight loss, which will delight a woman.
After losing weight, the following processes improve:
- sexual desire and libido;
- the menstrual cycle is restored and ovulation occurs;
- the ability to get pregnant and successfully carry a child;
- The appearance of the body and skin improves, acne and acne may disappear.
To achieve the best results, the patient should be comfortable, the diet should not cause negativity and unnecessary stress.
Forecast and prevention of polycystic ovary syndrome (PCOS)
The issue of prevention and prognosis of PCOS depends entirely on how ready the woman is for pregnancy and whether she wants to get rid of infertility. In many ways, it is also important how timely treatment for PCOS is started. Experts say that polycystic ovary syndrome in the early stages can be cured quite easily if treatment is carried out in a timely manner. Therefore, in such cases the prognosis is usually favorable. As for prevention, a woman needs to carefully monitor any changes occurring in her body, and also not forget about the timely fight against excess weight.
Who treats PCOS
A gynecologist or endocrinologist can treat PCOS with diet and other methods.
Endocrinologist Georgy Nikitich Romanov treats polycystic ovary syndrome in women in his medical practice. This specialist conducts paid online consultations with patients, interprets diagnostic results, advises on nutrition, medications, etc. Romanov Georgy is a candidate of medical sciences with more than 20 years of work experience. To schedule an online consultation with him, click here.
How do the symptoms appear?
Although a large percentage of the fair sex suffers from polycystic ovary syndrome, some of them may not even be aware of the presence of this disease. Everything is related to the great individuality of symptoms, which can manifest themselves in different ways.
The most common reasons to raise the question of polycystic disease are the following manifestations:
- disrupted menstrual cycle (too scanty or, conversely, heavy bleeding, lack of a stable cycle, excessively short or long cycle (according to the latest standards, it is less than 21 and more than 38 days), a gradual increase in the time interval between bleeding);
- pain in the lower abdomen, groin, lower back. More often of a pulling nature, periodic at first, and then can develop into permanent ones;
- a sharp increase in body weight while maintaining diet and physical activity, obesity;
- the appearance of pimples, acne, increased oiliness of hair and skin due to activation of the sebaceous glands;
- increased hair growth on a woman’s face and body in areas unusual for her;
- failure to conceive in the presence of regular unprotected sexual intercourse for one year or longer.
The totality of these symptoms or part of them may also be a sign of other hormonal and reproductive diseases. However, such a kit allows the gynecologist to make a preliminary diagnosis and prescribe additional examinations to diagnose polycystic ovary syndrome or another disease.
With polycystic disease, pregnancy followed by miscarriage is considered a common occurrence. A miscarriage itself implies a specific treatment for the consequences, but if the same situation is repeated repeatedly, we may be talking about this particular disease.
conclusions
The diet for polycystic ovary syndrome should be prepared by a specialist based on the patient’s individual parameters. It should be comfortable and varied. PCOS is not cured in a month - it is a long, painstaking work of the patient on himself and his daily habits. A diet for PCOS not only helps reduce the symptoms of the disease and restore the woman’s hormone balance, but also improves her appearance: the body becomes toned, physical activity and endurance increase, problems such as brittle nails, hair loss, constant fatigue, apathy, etc. .
PCOS treatment
Treatment of PCOS depends on the phenotype and is aimed at providing palliative care, normalizing metabolism and the menstrual cycle. The treatment package is selected jointly by a gynecologist and an endocrinologist.
, and success largely depends on the patient’s compliance with recommendations, rational nutrition (diet) and maintaining a healthy lifestyle.
Correction of lipid metabolism disorders in PCOS using metformin
, lipid-lowering drugs and vitamins is indicated for all patients (including those who are not overweight) for the treatment of infertility and is effective in almost 90% of cases, even when conservative and surgical treatment did not help.
Combined oral contraceptives (COCs) for PCOS
If you have polycystic ovary syndrome, you can and should
take combined oral contraceptives (COCs).
Moreover, if you do not drink them and are not yet planning a pregnancy, most likely your doctor will prescribe COCs for the treatment of PCOS
, since COCs allow you to control the cyclicity of the menstrual cycle and prevent endometrial hyperplasia.
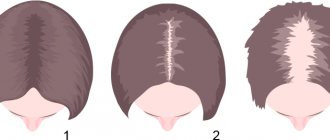
Usually a COC with an antiandrogenic effect
, so the patient also receives treatment for the clinical manifestations of hyperandrogenism (hirsutism, baldness, acne).
The main concern is the association between COC use and the development of venous thrombosis, and women with PCOS and overweight are at increased risk of thromboembolic complications. However, the absolute risk of such a complication remains quite low.
You can make an appointment with a gynecologist by calling: +7
And
+7
Diagnosis and treatment of polycystic ovary syndrome
If polycystic ovary syndrome is suspected, a specialist will definitely examine the patient and ask about weight changes and the last menstruation. To clarify the diagnosis, laboratory diagnostics are prescribed, which includes a blood test, mammography of the mammary glands, ultrasound of the pelvic organs and other research methods.
Therapy for Stein-Leventhal syndrome is aimed at eliminating the individual problems of each patient, for example, obesity, infertility, acne, hirsutism (excessive hair growth). To regulate the menstrual cycle, birth control pills can be prescribed; they reduce the level of androgens produced, thereby giving the woman’s body a break from the effects of estrogen. This therapy will minimize the risk of developing oncology (endometrial cancer), but it is only suitable for patients who are not planning pregnancy in the near future.
If diabetes mellitus and polycystic disease are diagnosed at the same time, then drugs that lower insulin levels must be prescribed; they will improve the patient’s condition and help ovulation. If you are overweight, a special diet is indicated, after which the reproductive function should resume. In cases where conservative therapy has failed, ovulation is stimulated through pelvic laparoscopy.
Surgery is effective in 90% of cases, but its effect is short-lived. Laparoscopy helps normalize ovarian function and achieve ovulation. Often, after surgery, hormonal treatment becomes more effective, and the patient gets rid of the problem of infertility.
For timely diagnosis and treatment of polycystic ovary syndrome, contact medical