What is nutritional obesity
If a person has eating disorders in the direction of constant overeating, carbohydrate and fat metabolism gradually slows down in the body, which leads to weight gain. When the extra kilograms become not 5 or 10, and all incoming carbohydrates turn exclusively into fat, which goes into the subcutaneous tissue and envelops the internal organs, doctors diagnose “obesity”. The label “alimentary-constitutional” or “exogenous-constitutional” means a direct connection between disrupted eating behavior and the appearance of excess weight.
Symptoms
Manifestations of obesity depend on the severity. Main symptoms:
- constant overeating, increasing the amount of food consumed over time;
- weight gain and corresponding appearance;
- hypertension;
- skin rashes caused by increased sebum secretion;
- hyperhidrosis;
- dyspnea;
- apnea, sleep disorder;
- crepitus and joint pain due to increased load;
- increased concentration of glucose in the blood, which can result in the development of diabetes mellitus - there is even an expression: “full of sugar”;
- deterioration in the performance of internal organs;
- allergic reactions due to the fact that the liver cannot cope with its work;
- deterioration of immunity;
- psycho-emotional instability, development of complexes.
In children at an early age, motor skills are formed late, constipation, allergies, and a tendency to constant colds appear. By adolescence, metabolic syndrome develops (impaired all types of metabolism), insulin resistance (inadequate body response to insulin - both its own and those coming from outside), hyperlipidemia (high concentration of cholesterol and triglycerides), dismetabolic nephropathy (impaired kidney function and structural changes ).
Reasons for development
The mechanism for the appearance of this disease is simple - under the influence of certain factors, the body ceases to correctly distribute the nutrients entering it, preferring only to store them. This is how excess weight is formed, which, in the event of serious failures, is fraught with the appearance of fat around the internal organs, including the heart. The factors that give rise to nutritional-constitutional obesity can be both external in nature - something that is easy to fight, and internal: congenital pathologies, etc. Based on them, doctors divide the disease into:
- primary;
- secondary.
External factors
Exogenous causes of figure problems in medical practice are more common than endogenous ones, especially in modern people who are forced to rely on work rather than on health. The main factor provoking weight gain here is an eating disorder associated with physical inactivity (often a sedentary lifestyle and lack of time for physical activity). Provocateurs of alimentary-constitutional obesity can be:
- the habit established in childhood of eating “first course, second course and compote”, which persists into adulthood - this leads to a serious excess of daily caloric intake, since nutrition covers several times the natural needs of the body;
- abuse of sources of simple carbohydrates and fats - they inhibit metabolic processes and contain “empty” calories;
- features of national cuisine (and food traditions) - this is especially noticeable among eastern peoples.
Internal factors
Endogenous causes are more difficult to both identify and eliminate, and they can be combined with exogenous ones, especially when it comes to mental illness and nervous disorders. Thus, during depression, there is a pathological craving for sweets (especially in women), which can gradually become permanent and be one of the reasons for alimentary-constitutional excess weight gain. However, there are a few more points that should not be missed:
- improperly functioning, due to pathology, saturation centers of the hypothalamus and endocrine glands provoke eating disorders;
- diseases of the endocrine glands, thyroid gland (often obesity of the alimentary-constitutional type is diagnosed in women with thyrotoxicosis);
- a combination of genetic factors - hereditary obesity and congenital problems of metabolic processes: if their speed is underestimated, the body begins to store even relatively small portions of fat (and slight excesses of the norm) in reserve;
- the structure of adipose tissue, which contains an excess number of adipocytes;
- hormonal imbalances (especially common in women during menopause and pregnancy).
Causes
If a person does not take pharmaceuticals that promote weight gain, does not suffer from metabolic disorders, endocrine pathologies, or nervous disorders, excess body weight is associated with lifestyle. Such people prefer high-calorie foods, sweets, fatty foods, and “fast” food. Many people have limited movements due to specific “sedentary” work in offices.
The very term “exogenous-constitutional” obesity reveals the causes of the disease. This implies the presence of exogenous (external) factors, such as lifestyle, and constitutional (related to the body) internal factors.
Exogenous causes:
- Constant overeating, when the number of calories taken in significantly exceeds the calories expended.
- Eating high-calorie foods, fast carbohydrates, foods with a lot of artificial colors that affect metabolism and the functioning of the digestive system.
- Food for the night. To process carbohydrates, you need insulin produced by the pancreas. The pancreas “rests” after 7 p.m., which is why the last meal should be no later than 6–7 p.m. Gastric enzymes are not produced at night or are synthesized in insufficient quantities to fully process food. Food consumed at night “forces” the organs of the gastrointestinal tract and endocrine system to work with great overload, which leads to rapid wear and tear of the system. If compensatory mechanisms are activated at a young age, in adults this leads to a real disaster. Most of the food is simply not digested overnight and remains unchanged in the stomach until the morning. This is another reason not only for excess weight, but also for poor sleep, when a person gets up in the morning unrested.
- There is no diet and culture, which causes the emergence of incorrect eating habits.
- Lack of physical activity or inactive lifestyle. The body requires much fewer calories per day for normal functioning.
Endogenous causes:
- Hormonal imbalance. Physiological hormonal imbalance occurs in adolescence with intense puberty, in pregnant women and nursing mothers, during menopause, and in men with age when testosterone production decreases. Hormonal imbalance is observed in many diseases, including obesity.
- Pathologies of the endocrine glands (dysfunction of the hypothalamic-pituitary system, diabetes mellitus, pituitary tumors, neoplasms and inflammation of the ovaries in women and testicles in men, genetic abnormalities, others).
- Mental disorders.
- Regular stress, as a result of which the habit of “eating” unpleasant situations has developed. In such cases, a person usually does not realize what and when he eats.
Nutritional obesity is diagnosed more often in women (75%) than in men.
Nutritional obesity as a risk factor
The cause of nutritional obesity in children is most often a hereditary factor, when one or both parents suffer from excess weight. The probability of developing pathology in a child is 50% if only the mother is obese, 38% if only the father is obese, 80% if both parents are obese.
In second place for reasons is energy imbalance associated with the discrepancy between consumed and expended calories, lack of physical activity, the habit of eating high-calorie foods, eating near the TV or computer, and ignoring physical education lessons in educational institutions. Children who spend half the day in a sitting position at school are accustomed to snacking on buns and sandwiches during breaks, the calories from which do not have time to be processed and absorbed by the body during the day.
At risk are infants born weighing more than 4 kg and bottle-fed children. Usually mothers “feel sorry” for their children, feed them high-calorie infant formula, and violate the feeding rules.
Obesity in children often occurs as the body's response to a stressful situation. For example, when entering school or transferring to another educational institution, moving to another city or country where there is no familiar environment, after the death of a loved one.
Obesity of alimentary-constitutional origin
How excess weight will be distributed depends on the type of disease, which is determined by the prerequisites for its occurrence. So, in people suffering from polycystic ovary syndrome, fat deposits are located in the abdomen, and in women who have problems with thyroid hormones, on the hips and in the pelvic area. In total, official medicine distinguishes 3 types of deposits:
- android (male);
- gynoid (female);
- combined.
Android type
Male type obesity is easy to determine - the main areas of deposits are the armpits and the entire abdominal area. Experts call a subtype of android nutritional weight gain abdominal weight gain, popularly known as a “beer belly,” which is dangerous due to the accumulation of fat around the internal organs of the abdominal cavity. During diagnosis, abdominal fat distribution can be detected if the patient's waist circumference is more than 88 cm for women and 102 cm for men.
Gynoid type
The classic variant in women is when excess body weight is observed mainly in the lower abdomen and hips. The remaining zones also increase in volume, but not so clearly. Often, the gynoid type of alimentary-constitutional obesity is associated with impaired ovarian function and excessive production of sex hormones (mainly prolactin due to a lack of testosterone). During menopause, most women also gain weight according to this pattern, but they do not always reach a dangerous stage.
Combined
If the person who has been diagnosed observes excess weight, distributed relatively evenly across all areas, this is a combined/mixed type of disease. The figure takes on the contours of an apple, the amount of fatty tissue is especially high on the stomach, hips and upper torso. This option is more dangerous than the gynoid and android type, since the risk of complications in the form of concomitant diseases (especially type 2 diabetes) is very high.
Classification
Obesity is classified according to severity:
- Obesity of the 1st degree is the initial phase of the disease, characterized more by aesthetic problems than physical ones. BMI (body mass index) is 30–34.9. A person is just beginning to “grow” with fat. Slightly, but noticeably, the waist and hips increase in volume. Slight shortness of breath and sweating, fluctuations in blood pressure begin to appear, but all this does not yet bother the patient. Treatment at this stage is highly effective, allowing you to completely get rid of the disease, but rarely does anyone resort to help at the first stage.
- Obesity 2 degrees - excess weight is clearly visible, BMI 35–39.9. Problems arise in performing habitual physical activities, which become increasingly difficult to do. Usually at this stage people pay attention to their well-being and begin to take measures to get rid of the pathology.
- Obesity 3 degrees - pronounced changes in appearance, BMI 40 or higher. A person suffers from intense shortness of breath; walking up stairs or uphill becomes a real problem. At the third stage, internal organs suffer, biochemical processes are disrupted, hormonal levels change, glucose levels rise to significant levels, persistent hypertension and psychological disorders appear. Treatment is ineffective.
There are three types of third degree obesity:
- Male type (android) - fat deposition on the abdomen, back, armpits, and lower back.
- According to the female type, fat is deposited in the lower abdomen, on the hips, buttocks, and chest.
- Mixed - fat accumulates evenly throughout the body.
With hormonal disorders, women store fat according to the male type, and in men - according to the female type.
Obesity in children and adolescents can be primary or secondary.
Primary:
- Exogenous-constitutional - associated with genetic predisposition.
- Nutritional – caused by improper diet and lifestyle. It is more often observed in children under three years of age, at 5–7 years of age, and at 12–16 years of age.
The secondary form is caused by pathologies of congenital or acquired origin.
There are 4 degrees of obesity in childhood:
- The first is that your weight is 15–24% more than normal.
- The second - by 25–49%.
- The third - by 50–99%.
- The fourth is 100% or more.
The first and second degrees are diagnosed in 80% of children; grade 4 obesity is extremely rare.
Obesity by BMI
Nutritionists prefer to determine how far the problem has gone by calculating the percentage deviation from the norm. Based on this, 4 stages of the disease are distinguished, where the last is an increase in weight by 2 times or more from that accepted as the norm for a particular physique and age. Doctors point out to patients that:
- There is no point in counting the number of extra pounds without reference to individual parameters.
- There are several methods for assessing BMI: a number of specialists classify figures up to 30 units (range from 25 to 30) as the pre-obesity stage, and someone already with 27 units establishes the first degree.
1st degree
If the proportion of excess weight does not exceed 29%, doctors diagnose exogenous-constitutional obesity of the 1st degree. When calculating body mass index, these will be values of 27.6-30 units if a person is in the age category from 18 to 25 years, and values of 28.1-31 units for persons over 25 years of age. However, here you need to make allowances for the individual physique: for those who have thin bones (asthenic type), these numbers need to be reduced by 10%.
2nd degree
If the normative weight indicators are exceeded by 30-49%, doctors diagnose “exogenous-constitutional obesity of the 2nd degree.” This period is characterized by an increase in BMI to 30.1-35 units in people under 25 years of age and to 31.1-36 units in those over 25 years of age. Symptoms of this condition include the appearance of shortness of breath when walking and the formation of folds on the abdomen. Mostly people over 50 years of age face the 2nd degree.
3rd degree
In some sources, the last stage of this disease is called the 3rd degree, but doctors prefer to separate it from the 4th, where the patient is completely incapacitated. Alimentary-constitutional obesity of the 3rd degree is an excess of weight by half or more from normal (up to 99%), and according to the body mass index these are values of 35.1-40 and 36.1-41 units for persons aged 18-25 years and over 25 years old.
4th degree
The last stage is accompanied by visceral fat - the most dangerous of all; it affects all internal organs and systems. In it, a person loses his legal capacity, cannot move normally, and his activity is reduced to zero. The excess of normal weight is more than 100%, the body mass index in people under 25 years of age is beyond 40.1 units, and in those over 25 years of age it is more than 41.1 units.
Rules for determining BMI
To correctly assess the situation and find out the degree of obesity, an individual approach to each patient is necessary.
First of all, you need to determine your body mass index; this is not difficult to do:
- first we determine the person’s height in meters and square it;
- Determine body weight and divide it by the resulting number.
A variant of the norm is considered to be an indicator that will not go beyond such values - 18.5 - 24.9. In such a situation, the risk of health problems is equal to zero.
If the indicator is from 25 to 29.9 this indicates overweight. Disorders in the functioning of the body will be observed when the threshold of 27 units is exceeded.
A BMI from 30 to 34.9 indicates first-degree obesity, from 35 to 39.9 – second-degree obesity. This situation requires serious treatment. An indicator above 40 units indicates obesity of the 3rd degree, people will have a full figure, and the presence of secondary diseases will be observed.
Level 4 obesity is indicated by an indicator exceeding 50 units. The fourth stage of the pathology is characterized by a severe course and serious health problems.
Accompanying illnesses
If you do not start treating the disease at the initial stage, later it will become more difficult to deal with the problem, since a lot of pathologies associated with changes in the functioning of internal organs will be added to it. Alimentary-constitutional weight gain, especially in the last stages, is not only an aesthetically unpleasant phenomenon, but also a threat to health, since it is complemented by:
- hypertension, which in old age can even be fatal;
- diseases of joints that cannot withstand the load;
- diabetes mellitus – against the background of obesity, there is a complete loss of the response of peripheral tissues to the hormone insulin, which has a negative effect on all systems of the body;
- ischemia, which can give the green light to other diseases of the cardiovascular system;
- atherosclerosis - the appearance of plaques on the vascular walls is fraught with blocking blood flow and rupture of the vessel.
Forecasts
The most favorable prognosis is for grade 1 obesity. If you start timely treatment and do not start the process, you can forget about the disease for a long time or forever. Obesity of the 2nd degree has a favorable prognosis, provided timely measures are taken, but coping with the problem is more difficult.
Stages 3 and 4 are dangerous for the development of various diseases, dysfunction of organs and systems. The following complications are possible:
- atherosclerosis;
- diabetes mellitus type II;
- hypertension;
- angina pectoris, ischemia;
- cholelithiasis and urolithiasis;
- chronic cholecystitis;
- fatty hepatosis, cirrhosis;
- constipation, hemorrhoids;
- bulimia, anorexia;
- apnea, insomnia;
- inferiority complexes, depression, self-isolation, asocialization;
- diseases of the musculoskeletal system;
- hormonal imbalances and related menstrual cycle disorders;
- infertility;
- sexual dysfunctions, impotence in men.
It is easier to stop the development of the pathological process at an early stage and return to a healthy life before irreversible consequences arise.
Diagnostic methods
You can conduct an initial check to determine the presence or absence of a large amount of fatty deposits that pose a health threat even at home - some of the diagnostic methods do not require the help of a specialist. However, to obtain an accurate diagnosis, especially when it comes to nutritional weight gain, which is secondary, you should consult a doctor. Often used to make a diagnosis:
- BMI calculation;
- assessment of the thickness of the abdominal fold;
- psychodiagnostic method.
Body Mass Index Calculation
The basic way to find out whether a large amount of excess weight is present is to find out your body mass index (abbreviated as BMI). This technique is considered not ideal, since it does not take into account the individual characteristics of a person’s constitution, but it helps with a high probability to determine the presence or absence of serious problems with the figure. The calculation scheme is simple: weight (kg) must be divided by height (m) squared. The resulting number will be the desired index. Afterwards it is compared with standard indicators.
Measuring the thickness of the abdominal fold
A popular method of bodymetry is to check the degree of fatness by the thickness of the fold located at the level of the navel on the side, or in the area of the front wall - you need to step back 5 cm from the navel. You can talk about excess body weight if the thickness of the tuck is more than 3 cm. Doctors perform a check with a special tool - a caliper, but the same manipulations can be done at home, with your fingers: thumb and forefinger.
Psychodiagnostics
Since nutritional-constitutional obesity is often based not so much on hormonal disorders or hereditary factors, but on eating disorders, to make a diagnosis, the doctor can conduct psychoanalytic diagnostics. It does not allow one to assess the extent of the disease, so it cannot be used alone, but it helps to more accurately establish the reasons that led to it and outline possible ways to solve the problem.
1.General information
Degeneration, dystrophy, atrophy are close synonyms or, more precisely, different phases of the degeneration of living tissue in conditions when its cells do not receive enough nutrients, bound oxygen, essential microelements and vitamins from the bloodstream for a long time. The tissue performs its functions worse and worse, decreases in volume and, in fact, slowly dies as an increasing number of cells gradually die with insufficient renewal and replenishment.
In this case we are talking about a similar process on the scale of the entire organism. The word “senility” translated from Greek means withering, drying out; “dystrophy”, in a broad sense, is a malnutrition, malnutrition (this may also include the vital processes of the cell, the nutrition of the tissue, and the metabolism of the entire organism as a whole).
Thus, nutritional, or nutritional insanity, nutritional dystrophy is a very dangerous state of extreme exhaustion that occurs as a result of nutritional deficiency. In the English-language literature, the specification “nutritional” is usually not used, and marasmus is meant as one of the types of protein deficiency, in which the processes of energy metabolism suffer mainly; Other types are cachexia, kwashiorkor, and hospital fasting. Thus, in Western sources, marasmus is considered a somatic status in which body weight is less than 62% of normal values for a given height; according to these sources, a similar degree of exhaustion is most often observed in children under the age of 1 year, although it can occur at any age and under the influence of various causes (cancer diseases, severe endocrine pathology, fibrosing processes and other factors that can block the absorption and assimilation of nutrients) .
However, in the domestic literature, nutritional insanity (dystrophy) is considered as a separate pathology and is defined more clearly - as a condition associated specifically with prolonged general starvation. The term itself entered the Russian-language medical lexicon during the Leningrad blockade, which in itself says a lot.
A must read! Help with treatment and hospitalization!
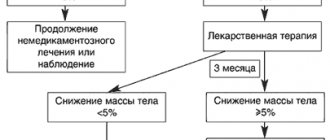
Treatment of nutritional-constitutional obesity
If the presence of several (up to ten) extra kilograms can be dealt with exclusively by diets or simply removing chocolate and fast food from the diet, then when it comes to metabolic syndrome and weight gain of the alimentary-constitutional type, it is necessary to draw up a full course of therapy that will follow such diagram:
- Discovering the causes of eating problems with a psychologist.
- Changing your diet together with a nutritionist.
- Introducing light/moderate physical activity under medical supervision.
- Prescribing medications that correct metabolic processes, appetite, insulin (if necessary), etc.
Diet food
It is advisable to adjust the menu with a nutritionist who will calculate your individual calorie needs. Alimentary-constitutional obesity requires giving up sources of simple carbohydrates and partially reducing the share of complex carbohydrates - removing potatoes, reducing the frequency of eating cereals and all types of bread. Meals are fractional: portions are small and frequent. Proteins and carbohydrates are not combined. At the last stage of the disease, doctors recommend the following daily regimen:
- up to 300 g of lean meat;
- up to 300 g of cottage cheese;
- up to 400 ml of lactose-free milk;
- about 700 g of vegetables (without legumes);
- 500-700 g of fruit (unsweetened);
- no more than 50 g of black bread.
Physical exercise
People who have been diagnosed with nutritional-constitutional obesity are not prescribed serious sports - they are not even allowed to go on a treadmill, since the joints and spine will not withstand such a load. However, physical activity must be present in the therapeutic regimen: at first it is represented only by walking, lasting 15-30 minutes at a calm pace. Afterwards, their duration is increased, and at stages 1-2 of the disease, therapeutic exercises can be prescribed.
Drug treatment under medical supervision
The use of medications in persons with alimentary-constitutional obesity is not considered mandatory unless there are pronounced concomitant diseases (especially those affecting the thyroid gland and liver). Most medications are symptomatic in nature:
- Medicines that control appetite (Avikol, Fepranon) are used for eating disorders.
- Metabolic agents (Xenical) - they accelerate metabolic processes.
- Regulators of neurotransmitter metabolism (Phenytoin) are prescribed to those diagnosed with hypothalamic obesity.