Obesity
– this is not an aesthetic (or cosmetological) problem, but a chronic disease, manifested primarily through the accumulation of excess fatty tissue in the body. Gaining excess weight is often a consequence of metabolic disorders, and it itself is the cause of various pathologies. Thus, excess body weight contributes to the development or aggravates the course of cardiovascular diseases, joint diseases, as well as diabetes mellitus, cholelithiasis, gout, and leads to sexual dysfunction. Therefore, the problem of excess adipose tissue is complex, and trying to cope with obesity on your own - with the help of advice from “knowledgeable” people - is sometimes downright dangerous. It is necessary to fight excess weight under the guidance of a doctor.
What is considered obesity and how does it happen?
To determine the deviation of body weight from the norm, the body mass index
– BMI. It is calculated as the ratio of body weight (in kilograms) to a person's height (in meters) squared and measured in units of kg/m².
BMI is used to characterize people aged 18 to 65 years. If the BMI is less than 18.5 kg/m², underweight is diagnosed. Normal range: from 18.5 to 24.9 kg/m². A BMI in the range of 25-29.9 kg/m² indicates the presence of overweight and obesity. This is not a disease yet, but a signal that a person should take control of his weight. With a BMI above 30 kg/m², obesity is diagnosed: from 30 to 34.9 kg/m² - I degree, from 35 to 39.9 kg/m² - II degree, over 40 kg/m² - III degree. As the degree of obesity increases, the risk of developing concomitant diseases increases - from high to extremely high, that is, concomitant diseases become simply inevitable.
There are also different types of obesity
:
Abdominal
(from the Latin word abdomen - “belly”) - when excess fatty tissue forms in the abdomen or upper torso.
This type of obesity is also called “male” obesity, since it is more common in men, or “apple” obesity. Abdominal obesity increases the risk of cardiovascular disease. Femoral-gluteal
- the lower type of obesity, more common in women. It is also called pear-shaped obesity. The lower type of obesity is often accompanied by diseases of the spine, as well as joints and veins of the lower extremities.
Mixed
when excess fat tissue is distributed evenly throughout the body.
You can determine the type of obesity by measuring your waist and hips. If a man has a ratio of waist circumference to hip circumference greater than 1.0 (WC/HR>1), then the abdominal type is diagnosed. In women, the abdominal type is established when WC/VT>0.85.
Waist circumference is also used in diagnosing obesity. If in men WC>102 cm, and in women WC>88 cm, then this is abdominal obesity. However, already with WC>94 in men and WC>80 cm in women, the risk of developing type 2 diabetes and cardiovascular diseases increases.
Obesity treatment can be carried out at the 24-hour Therapeutic Hospital on Barrikadnaya as part of the Weight Loss treatment and health program. The course of therapy can range from 1 to 10 days.
Monogenic defects and endocrine imbalance
We found that dysfunction of the leptin-melanocortin pathway leads to dysregulation of hunger/satiety and is a direct cause of obesity, but increased appetite is not the only problem. The absence of leptin or leptin signal is accompanied by the following disorders in the endocrine system:
- Activation of the hypothalamic-pituitary-adrenal axis with increased cortisol synthesis.
- Decreased activity of the thyroid gland with symptoms of hypothyroidism.
- Suppression of reproductive function and synthesis of sex hormones with signs of hypogonadism.
- Decreased secretion of growth hormone.
How the endocrine disorders listed above affect body weight are described in the following sections of the article. In short, even one of these disorders can cause morbid obesity, and complex hormonal dysfunction is guaranteed to lead to significant weight gain.
A review of the leptin-melanocortin pathway shows that the causes of obesity are not simple. There are factors that medicine knew nothing about a couple of decades ago. Every year, new data emerges that shed light on the true causes of obesity associated with inherited defects and genetic disorders of the regulation of eating behavior.
Causes of obesity
Obesity can be caused by diseases of the endocrine system or digestive organs. However, the main reason is that a person receives more energy from food than his body expends.
Factors contributing to obesity
:
- eating disorder (habit of eating a lot);
- stress (it is human nature to “eat up” stress, compensating for the negative with positive emotions that arise when eating delicious food);
- insomnia (while awake at night, a person is inclined to organize an extraordinary meal, increasing daily calorie intake);
- sedentary lifestyle;
- quitting smoking (the usual cigarette is replaced by sweets, nuts, seeds, etc.);
- family tradition;
- alcoholism;
- taking certain medications;
- pregnancy and childbirth.
Monogenic obesity
What is monogenic obesity? Many readers encounter this term for the first time, so it requires a separate explanation.
Monogenic obesity is a disease caused by a mutation in the gene encoding one of the elements of the leptin-melanocortin pathway for the regulation of hunger and satiety. Monogenic obesity is accompanied by bulimia and progressive weight gain.
In this definition, the reader without a medical education has already encountered several incomprehensible terms. To make everything clear and understandable, what follows is a detailed description of the terms in a simplified form.
What is the leptin-melanocortin pathway?
One of the key regulators of appetite, hunger and satiety is the leptin-melanocortin pathway. The main components of this path:
- Leptin is a hormone in adipose tissue that is produced in response to food intake.
- Melanocortins are CNS mediators that stimulate satiety centers and suppress hunger centers in the brain. Melanocortins are key regulators of eating behavior and energy balance in our body.
There is a direct connection between leptin and melanocortins: leptin enhances the synthesis of melanocortins. The process of regulating eating behavior is simplified as follows:
- Eating increases leptin synthesis.
- Leptin acts on specific receptors in the hypothalamus and stimulates the synthesis of melanocortin.
- Melanocortin activates satiety centers and suppresses hunger centers.
- The person feels full and stops eating.
This is a simplified scheme for regulating eating behavior, since more factors are involved in the process. For example, the secretion of melanocortin is also stimulated by hyperglycemia, insulin, and other hormones. Leptin acts on AgPR/NPY neurons, the activation of which increases the feeling of hunger. Leptin blocks these neurons, thereby having an anorexigenic effect (reduces appetite).
Reference.
AgPR/NPY neurons: cells of the central nervous system, the activation of which is accompanied by an orexigenic effect (increased appetite).
What does this have to do with the causes of obesity?
The most direct. Scientists have proven that there are several key elements in the functioning of the leptin-melanocortin system; a genetic defect in one link leads to hyperphagia (overeating) and malignant obesity. Genetic defects affecting one single gene are called monogenic.
What defects can lead to the development of monogenic obesity?
Mutations in genes encoding can lead to the development of morbid obesity:
- leptin (LEP);
- leptin receptors (LEPR) in brain cells;
- receptor tyrosine kinase type 2 (NTRK-2);
- pro-opiomelanocortin (POMC);
- melanocortin receptors (MC4-R).
All of the factors listed above are important elements of the leptin-melanocortin pathway for the regulation of eating behavior. In fact, there are more links in this chain, but the article provides only the key elements, otherwise, instead of popular science material, the result will be scientific material that is too difficult to understand.
So, the cause of obesity, as well as the true cause of overeating, may be a mutation in the gene responsible for the synthesis of leptin in fat cells. A defect in the gene encoding leptin receptors in POMC neurons and AgPR/NPY neurons of the brain will lead to similar results: leptin is produced in the patient’s body, but the centers of the brain are insensitive to it.
The cause of obesity may be a defect in the receptor responsible for intracellular signal transmission. The fact is that leptin receptors are located on the surface of POMC neurons that produce melanocortin. Intracellular transmission is carried out with the participation of tyrosine kinase, the defect of which leads to dysfunction of the entire leptin-melanocortin pathway.
The cause of obesity may be a monogenic defect in the gene encoding proopiomelanocortin itself in POMC neurons. This mutation leads to the fact that melanocortins are simply not formed. There is leptin, there are receptors, but the system does not work due to the lack of an intermediate component. Result? Uncontrolled appetite and obesity.
Finally, a mutation in the melanocortin receptor gene MC4-R may be the cause of obesity. Melanocortin interacts with these receptors. If there is a defect in the MC4-R receptors, signal transmission to the saturation centers becomes impossible. The result of a monogenic mutation will also be bulimia with progressive weight gain.
Methods for diagnosing obesity
Treatment of obesity begins with a complete health examination and identification of the cause of excess weight.
.
A set of diagnostic procedures is recommended, including methods such as:
Anthropometry
Anthropometry for obesity includes calculating BMI, measuring waist circumference and hip circumference, and assessing the thickness of subcutaneous fat using a caliper.
Bioimpedancemetry
Obesity can also be diagnosed using instrumental methods, primarily bioimpedance measurements. Using a special device, the electrical resistance of the body is measured, which makes it possible to calculate BMI, fat and lean mass, active cell mass, total body fluid, as well as separately intracellular and extracellular fluid.
Laboratory diagnostics
For obesity, a biochemical blood test is performed (indicators: blood glucose, glycated hemoglobin, cholesterol, LDL, HDL, creatinine, bilirubin, uric acid, gamma GT), as well as a hormone test (indicators: TSH, T4, leptin, insulin, vitamin D , prolactin, LH, FSH, testosterone, estradiol). Research data can be combined in a special profile “Weight Control”).
Ultrasound examinations
In case of obesity, ultrasound examinations of the abdominal organs, pelvic organs (in women, in men – prostate gland), and thyroid gland are performed.
More information about the diagnostic method
ECG
Obesity increases the risk of cardiovascular disease. An ECG will allow you to assess whether weight gain has affected your heart function. Additional research may be required if necessary.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Obesity with hypogonadism
Hypogonadism is a syndrome that develops when the secretion of sex hormones by testicular tissue decreases. The cause of primary hypogonadism is pathology of the testicles; secondary hypogonadism develops as a result of a decrease in the production of tropic hormones of the pituitary gland or releasing factors of the hypothalamus.
Obesity with hypogonadism develops according to the female type, with the predominant localization of excess adipose tissue on the hips, buttocks, and abdomen. The patient has poorly developed secondary sexual characteristics, often underdeveloped testicles and prostate gland. Many people do not grow hair on their body and face. A possible symptom is true gynecomastia. Libido is reduced, impotence develops.
Diagnosis of hypogonadism is based on a detailed analysis of the hormonal profile. Treatment is aimed at eliminating the causes of the disease.
Obesity Treatment Methods
The goals of treatment may vary. This:
- weight loss
(it is safe for the body to reduce weight by no more than 0.5-1 kg per week); - maintaining the achieved level of body weight
(after losing weight) and preventing its re-increase; - treatment of concomitant diseases
or reducing the risk of their occurrence.
When and which doctor should you contact if you are obese?
Obesity treatment is carried out by an endocrinologist. It is he who conducts the initial examination of the patient, gives directions for the necessary diagnostic tests, and, if necessary, refers to other medical specialists (gastroenterologist, gynecologist, urologist, neurologist, cardiologist, ophthalmologist). To change your lifestyle, sometimes you need to consult a psychotherapist.
Treatment for obesity is necessary if your BMI (body mass index) is more than 30 kg/m². But sometimes treatment should be started with a BMI>27 kg/m² if:
- You are planning a pregnancy;
- there is abdominal obesity (the ratio of waist circumference to hip circumference in men is more than 1, in women - more than 0.85);
- you suffer from type 2 diabetes mellitus or arterial hypertension;
- there is a hereditary predisposition to type 2 diabetes or arterial hypertension;
- increased blood cholesterol levels (threat of atherosclerosis);
- are concerned about diseases of the musculoskeletal system (joints, spine).
The obesity treatment complex includes:
Lifestyle change
Treatment of obesity will be ineffective without lifestyle changes. First of all, it is necessary to overcome eating habits that contribute to overeating, as well as increased physical activity agreed with the doctor.
Diet correction
It is necessary to limit daily energy intake to 1200-1500 calories. The transition to a diet must be carried out under the supervision of a doctor.
Drug treatment
If necessary, drug treatment can be carried out as prescribed by an endocrinologist.
Treatment of concomitant diseases
Treatment of concomitant diseases can be carried out both on an outpatient basis and, if necessary, in a day hospital.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Drug treatment of obesity in patients with metabolic syndrome
In recent years, the prevalence of obesity among the population has been steadily increasing in most countries of the world. Our country is no exception: according to the Endocrinological Dispensary of the Moscow Department of Health, the number of obese people has increased over the past 10 years among adults by 51%, among adolescents by 75% and by 66% among children.
Figure 1. Dynamics of carbohydrate metabolism parameters during 24-week therapy with Xenical
Figure 2. Dynamics of tissue sensitivity to insulin (Si) during therapy with Xenical
Figure 3. Dynamics of lipid metabolism parameters during 24-week therapy with Xenical
Figure 4. Dynamics of average 24-hour blood pressure monitoring during 24-week therapy with Xenical
Table. Dynamics of EchoCG parameters during therapy with Xenical
Figure 5. Dynamics of cerebral perfusion in patients with MS against the background of a decrease in body weight by 16 kg (14%) during 24 weeks of taking the drug Xenical
Figure 6. Orlistat affects all manifestations of metabolic syndrome
Of particular danger is the central type of obesity with predominant fat deposition in the abdominal region, which is associated with insulin resistance (IR), impaired carbohydrate and lipid metabolism, arterial hypertension (AH) and increased cardiovascular morbidity. All these disorders are pathogenetically interrelated and are combined into the concept of metabolic syndrome (MS). It has been established that the presence of MS increases the risk of developing type 2 diabetes mellitus (DM) by 3-6 times (6) and hypertension (9), and cardiovascular morbidity and mortality in people with MS is significantly higher compared to persons without it (4 ).
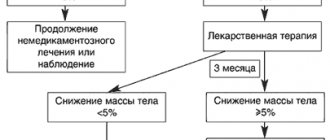
The primary and pathogenetically substantiated goal of therapy for patients with MS is measures aimed at treating obesity and normalizing metabolic disorders. Non-drug measures are aimed at reducing body weight, changing dietary patterns, giving up bad habits such as smoking and alcohol abuse, increasing physical activity, i.e. on the formation of a so-called healthy lifestyle. Non-drug treatment is more physiological, accessible and does not require large material costs; at the same time, significant efforts are required on the part of doctors and the patient himself, since this type of treatment requires additional time.
In some cases, it is necessary to add weight loss medications to non-drug methods of treating obesity. There are indications for their use, namely:
- body mass index (BMI) ≥ 30 kg/m2;
- or BMI ≥ 27 kg/m2 in combination with abdominal obesity, a hereditary predisposition to type 2 diabetes and the presence of risk factors for cardiovascular complications (dyslipidemia, hypertension and type 2 diabetes).
Medicines for weight loss are divided into groups of drugs with central action, peripheral action and various actions (growth hormone, androgens).
Most centrally acting drugs that reduce appetite were discontinued due to side effects, often leading to the death of patients, the most severe of which was the occurrence of severe pulmonary hypertension. These effects occurred, as a rule, due to the systemic action of these drugs.
The history of the creation and introduction into medical practice of “anorectics” - drugs to reduce appetite - is dramatic (7). The first drug proposed for weight loss was the well-known amphetamine. This was in 1938. But soon the adverse side effects of its administration became known - a pronounced stimulating effect on the central nervous system, as well as a withdrawal syndrome that occurs when stopping its use. Amphetamine is not currently used to treat obesity.
The next “black streak” in the history of the use of anorectics is associated with the epidemic of primary pulmonary hypertension (PPH), which broke out in the mid-1960s in Switzerland, Germany and Austria. It arose after the distribution of aminorex fumorate. PPH is one of the most severe cardiovascular diseases. Fortunately, this pathology is very rare - on average in 1-2 cases per million of the population, but when certain anorectics are prescribed, its frequency increases many times over. Thus, in the work of a group of American pulmonologists, it was shown that the incidence of PLH with the use of aminorex increases approximately 30 times.
In the 1980s and 90s, the drugs of choice for treating obesity were fenfluramine, drugs that affect serotonin metabolism, and phentermine, which has a stimulating effect on the sympathetic nervous system. The combination of phentermine and fenfluramine, the so-called fen-phen drug, was also popular. These drugs attracted attention due to their high efficiency and good tolerability compared to their predecessors. But, unfortunately, the stimulating effect on the sympathetic nervous system, as well as the toxic effect of high concentrations of serotonin, led to dysfunction and damage to the vascular endothelium, primarily the lungs, which was accompanied by an increase in vascular tone and the development of pulmonary hypertension. Fenfluramines, in addition, in some cases led to pathology of the heart valve apparatus (10). Several studies have also shown that fenfluramine may increase systemic pressure and heart rate (HR), both of which are unfavorable in patients with hypertension (2). The incidence of pulmonary hypertension with fenfluramine was significantly lower than with aminorex and, as a rule, side effects with these drugs developed after 6 months of continuous use. But the concerned medical community turned to regulatory authorities with a request to ban the sale of these drugs, and since 1997, their distribution has been prohibited in a number of countries, and in others the period of use is limited to 3-6 months.
Previous failures and the desire to have the safest and most effective drug possible forced scientists to take a different path - to create a drug with local rather than central action. The efforts of pharmacists were aimed at creating a medicine whose action would be local. Such a drug is Xenical (orlistat 120 mg), a drug for the treatment of obesity with a non-systemic effect.
In 2009, in the second revision of the VNOK recommendations for the diagnosis and treatment of MS, experts proposed the use of two drugs for the treatment of obesity. These are a peripherally acting drug - orlistat - and a centrally acting drug - sibutramine.
Sibutramine differs from its predecessors fenfluramine in that it has a lesser effect on dopamine metabolism and does not affect cholinergic processes. Taking sibutramine leads to a rapid onset of satiety and decreased appetite. However, the first studies showed that the use of sibutramine in people who do not suffer from hypertension may be accompanied by an increase in blood pressure by 3-4 mm Hg. Art. and an increase in heart rate. This property of increasing blood pressure and heart rate limited the use of sibutramine in patients with hypertension, MS and an increased risk of cardiovascular diseases.
In 2009, the randomized, double-blind, placebo-controlled SCOUT (Sibutramine Cardiovascular Outcomes Trial) study, which included more than 10,000 overweight and obese patients with diabetes or a history of coronary heart disease, peripheral artery disease or stroke, was completed. as well as with other cardiovascular risk factors. The study was designed to evaluate the safety of long-term use of sibutramine in this category of patients.
When analyzing the primary endpoints of this study (myocardial infarction, stroke, resuscitated cardiac arrest, or death), the rate was 11.4% in the sibutramine group and 10% in the placebo group. Thus, the risk of cardiovascular complications was significantly higher in patients taking sibutramine (p = 0.023) (5).
The data obtained in the SCOUT study are of great clinical importance, since patients with overweight and obesity have an inherently high risk of developing cardiovascular complications. Thus, in light of new data, the use of sibutramine for the treatment of obesity in patients with MS is contraindicated. The European Medicines Agency (EMEA) has completed a safety review of medicinal products containing sibutramine. The European Medicines Committee (CHMP) concluded that the risks of using these drugs outweigh the benefits and recommended suspending the license for their sale in the European Union.
As of January 21, 2010, sibutramine is prohibited for use in patients with a history of cardiovascular disease, as announced by the Food and Drug Administration (FDA). Based on new data from the SCOUT study, the FDA committee ordered new additional contraindications to be added to the instructions for use of the drug.
In Russia, the drug sibutramine is registered under the following trade names: Meridia (Abbot, Germany), Reduxin (Ozone LLC, Russia), Goldline (Ranbaxy, India), Slimia (Torrent, India), Lindaxa (Zentiva, Czech Republic).
Thus, doctors all over the world have in their arsenal the only safe drug for the treatment of obesity in patients with MS – orlistat.
Xenical (orlistat 120 mg) is a peripherally acting drug that inhibits the absorption of food fats in the gastrointestinal tract (GIT) due to inhibition of gastrointestinal lipases, key enzymes involved in the hydrolysis of food triglycerides, the release of fatty acids and monoglycerides. This results in about 30% of the triglycerides in food not being digested or absorbed, creating an additional calorie deficit compared to using only a hypocaloric diet. After discontinuation of orlistat, lipase activity is quickly restored. Orlistat does not affect other gastrointestinal enzymes and does not affect the absorption of carbohydrates, proteins and phospholipids. The drug has its own additional lipid-lowering effect, since, by suppressing gastrointestinal lipases, it reduces the amount of free fatty acids in the intestine and thereby reduces the solubility and absorption of cholesterol. Orlistat has been shown in a number of studies to reduce cholesterol levels to a greater extent than would be expected from weight loss alone.
Xenical has been used for the treatment of obesity for more than 11 years, during which time more than 100 clinical studies have been conducted, the results of which made it possible not only to evaluate the effectiveness and safety of the drug for the treatment of obesity based on the degree of weight loss, but also to evaluate its effect on cardiometabolic risk factors.
Patients receiving orlistat in combination with a hypocaloric diet lost 4.7 to 10.3 kg of body weight, while patients receiving placebo lost 0.9 to 6.4 kg (p
Numerous studies have been conducted to evaluate the effectiveness of orlistat therapy in patients with MS. Thus, according to these studies, it was revealed that therapy with Xenical led to a significantly greater reduction in the level of total cholesterol and the LDL cholesterol fraction compared to the placebo group. Also, in all comparative studies, a significant decrease in blood pressure was noted (8).
In the USA, a study was conducted of the effect of the drug Xenical on body weight and the state of carbohydrate metabolism in patients with type 2 diabetes who took sulfonylurea drugs. The results of this study showed that orlistat significantly reduced body weight in patients with diabetes and obesity (3). During orlistat therapy, the level of fasting glycemia significantly decreased and the concentration of glycated hemoglobin decreased. One of the most important results of this study was that patients taking orlistat had a reduced need for sulfonylurea drugs to compensate for diabetes.
In addition, analysis of data from this study showed that among patients with normal glucose tolerance while taking orlistat for 2 years, no new cases of type 2 diabetes were identified, while in the placebo group, type 2 diabetes developed in 1. 5% of cases. Impaired glucose tolerance was determined over time to be 2 times greater in the placebo group than in the orlistat group.
The results of the prospective, randomized, placebo-controlled XENDOS study involving 3304 obese patients confirmed the effectiveness and safety of long-term therapy (continuously for 4 years) with Xenical in obese patients. By the end of the fourth year of therapy, the level of LDL cholesterol decreased by 12.8%, and in the placebo group - by 5.1%. Systolic blood pressure in patients taking orlistat decreased by an average of 4.9 mmHg. Art. and diastolic by 2.6 mm Hg. Art., which was significantly higher compared to patients taking placebo (3.4 mm Hg and 1.9 mm Hg, respectively). The risk of developing type 2 diabetes decreased by 37% in the orlistat group compared with the placebo group (11).
The ability of orlistat to partially block the absorption of dietary fats was the basis for conducting a study to study the effect of its long-term use on the concentration of fat-soluble vitamins. His results showed that taking the drug for 2 years was accompanied by a slight change in the concentration of fat-soluble vitamins (A, D, E, K) and, on average, their levels remained within normal values. In addition, it was found that a decrease in vitamin concentration was observed only in the first month of treatment; subsequently, it remained unchanged until the end of the study. None of the patients in the study had symptoms of hypovitaminosis.
Laboratory and clinical signs of calcium metabolism disorders were also not observed during long-term use of orlistat (Xenical). Several studies have shown that there was no increase in osteoclast-osteoblast activity or decrease in bone mass with long-term administration of orlistat. Based on these observations, it was concluded that orlistat has no effect on metabolic processes in bone tissue.
Therapy with Xenical, as a number of studies have shown, does not lead to an increased risk of stone formation in the biliary tract. These adverse events occurred in only 1% of cases in both the orlistat group and the placebo group. A number of other studies found that the drug did not cause clinically significant disturbances in physiological processes in the gastrointestinal tract.
Clinical studies of the drug Xenical were carried out on a huge number of patients, more than 30,000 people participated in these studies, among them were patients with type 2 diabetes, impaired glucose tolerance and other multiple cardiovascular risk factors. In this regard, it is safe to say that at present this drug is the most widely and thoroughly studied drug for the treatment of obesity.
Positive experience of using Xenical in the Department of Systemic Hypertension of the Research Institute of Cardiology named after A.L. Myasnikov RK Scientific and Practical Training Center of the Ministry of Health of the Russian Federation in patients with MS once again confirmed its high effectiveness and safety for the treatment of patients with high cardiovascular risk (1). The purpose of this study was to study the effect of weight loss during orlistat therapy on parameters of carbohydrate and lipid metabolism, IR, daily blood pressure profile, left ventricular myocardial hypertrophy and cerebral perfusion state in patients with MS. The study involved 30 patients aged 39.9 ± 8.6 years with MS, average body weight was 116.5 ± 5.7 kg. All patients were prescribed Xenical at a dose of 120 mg 3 times a day with meals, and were given recommendations on a moderate hypocaloric diet with limited fat intake.
As a result of taking the drug Xenical for 24 weeks, it was possible to achieve a significant reduction in body weight, on average by 16 kg, or more than 14%, and this decrease was accompanied by a decrease in the severity of visceral obesity. Reducing body weight during therapy with Xenical led to a significant decrease in IR and improvement in carbohydrate and lipid metabolism. Fasting plasma glucose levels significantly decreased by 26% and postprandial levels by 29% (Figure 1).
There was also a decrease in hyperinsulinemia - initially elevated basal levels of insulin and C-peptide decreased by 54% and 32%, respectively, and their postprandial levels - by 38% and 7%, respectively. While taking the drug Xenical, there was a significant increase in the sensitivity of peripheral tissues to insulin, which was demonstrated by the results of an insulin-modified glucose tolerance test (Minimal model N. Bergman) (Figure 2).
Initially impaired lipid metabolism parameters significantly improved while taking Xenical. The level of total cholesterol significantly decreased by 12%, LDL cholesterol by 17.6%, the level of HDL cholesterol increased by 22%, and there was a trend towards a decrease in triglycerides (Figure 3).
Against the background of a decrease in body weight, increased tissue sensitivity to insulin and improved indicators of carbohydrate and lipid metabolism, blood pressure (both systolic and diastolic) significantly decreased both during the day and at night, and the daily blood pressure profile improved (Figure 4). The decrease in blood pressure as a result of weight loss may be mediated by a decrease in the increased activation of the SNS and the renin-angiotensin-aldosterone system. These effects are likely due to a decrease in the amount of FFA and an increase in tissue sensitivity to insulin along with a decrease in body weight.
After 24 weeks of therapy with Xenical in patients with MS and signs of left ventricular myocardial hypertrophy (LVMH), it significantly decreased against the background of a decrease in body weight, blood pressure and favorable metabolic effects (see table).
The decrease in LVMH while taking Xenical is probably due to a decrease in body weight, an improvement in the sensitivity of peripheral tissues to insulin, resulting in a decrease in hyperinsulinemia, which can probably play a significant role in the formation of LVMH. In addition, a decrease in blood pressure could also have a beneficial effect on the structural and functional state of the myocardium.
The initially reduced cerebral perfusion in patients with MS significantly improved due to a decrease in body weight, blood pressure, IR and improvement in carbohydrate and lipid metabolism (Figure 5).
Such a pronounced positive effect on the state of brain perfusion can most likely be associated with a decrease in IR, improvement in carbohydrate and lipid metabolism, which probably led to an improvement in hemostasis and blood rheology and caused an improvement in blood circulation not only in large, but also in microcirculatory vessels beds. In addition, the reduction in IR may have led to improved endothelial function and increased endothelium-dependent vasodilation.
Of the adverse events, patients observed only steatorrhea, which, as is known, occurs only when dietary fat intake exceeds 30%. Steatorrhea was a kind of “indicator” of excessive fat consumption, and this helped patients independently adjust their diet.
The high peripheral selectivity of the drug Xenical, the absence of systemic action and serious side effects, a significant decrease in body weight, which is accompanied by a decrease in blood pressure and a significant improvement in lipid and carbohydrate metabolism, which are serious cardiovascular risk factors, gives reason to recommend Xenical for use in cardiological practice. Due to the fact that this drug has a positive effect on all manifestations of MS (Figure 6), leveling them, Xenical can also be successfully used to prevent the development of MS in healthy overweight individuals.
Syndromic obesity
In popular materials devoted to the problem of being overweight, the term “genetic obesity” often appears. Typically, this term refers to a nonspecific set of hereditary factors that creates the prerequisites for the development of constitutional exogenous obesity. In other words, it increases the likelihood of weight gain when you increase your caloric intake.
Syndromic obesity is a more specific, scientific concept. It is characteristic of true genetic diseases, in which there is a gross violation at the level of gene complexes or entire sections of chromosomes.
An example of syndromic obesity is Prader-Willi syndrome, in which a fragment of the paternal chromosome is missing from the genome. Obesity develops in childhood. Children with this disease have an abnormally good appetite, but they grow poorly and develop disproportionately.
Syndromic obesity is also characteristic of the following genetic diseases:
- Alström syndrome.
- Down syndrome.
- Fragile X syndrome.
- Killian's syndrome.
- Cohen's syndrome.
- Carpenter's syndrome.
- Lawrence-Moon-Bardet-Biedl syndrome.
- Other genetic syndromes.
Hypothalamic obesity
Formally, hypothalamic obesity can be classified as a previous group, that is, endocrine obesity. The hypothalamic-pituitary structures are part of the endocrine system and are directly involved in regulating the functioning of the endocrine glands. However, the specificity of these forms of the disease makes it possible to place hypothalamic obesity in a separate category.
In hypothalamic obesity, the cause of hormonal imbalance is located at the level of the brain centers that regulate the function of the endocrine system. The cause of pathological changes may be traumatic brain injury, a tumor process localized in subcortical structures, a stroke, brain surgery, an infectious disease affecting the central nervous system. However, often the root cause of the disease cannot be determined.
Obesity due to medication use
Obesity can be caused by taking certain medications. Patients taking systemic corticosteroids face a high risk of weight gain. Medicines from this group are often prescribed for the treatment of autoimmune diseases: systemic lupus erythematosus, scleroderma, rheumatoid arthritis, and others.
Patients undergo hormonal therapy for a long time. The prescription of corticosteroids is explained by the powerful anti-inflammatory effect of these drugs. Stimulation of lipogenesis is a side effect of drugs that has to be tolerated, since the therapeutic effect is more important for patients with autoimmune diseases.
Obesity may be caused by other medications, such as antidepressants or oral hormonal contraceptives. Given the variety of contraceptives, if a side effect occurs, a woman should change the drug or choose a different method of contraception. The problem with antidepressants should only be solved together with your doctor.