“Space diet” by Sergei Sivokho: without denying himself anything, the comedian lost 42 kg in 3 months
Another dietary restriction for the purpose of instant weight loss without causing harm to health is a protein-free diet. It will not only get rid of excess weight, but also replenish the body with all the necessary vitamins and nutrients.
Why it is useful and whether it is worth sticking to it, we will consider further.
General rules
A low-protein diet is recommended for kidney disease, and there is a reason for this. The kidneys ensure the constancy of the internal environment of the body, since one of their functions is to remove toxins , allergens and metabolic end products ( creatinine , urea and bilirubin ).
Chronic renal failure , which is based on the death of nephrons, leads to loss of filtration function of the kidneys. The main causes of renal failure are chronic kidney diseases ( glomerulonephritis , pyelonephritis , nephrosclerosis , which are collectively called “chronic kidney disease”), diabetes mellitus and arterial hypertension . Despite treatment, renal failure is irreversible, progresses and eventually enters the terminal stage.
With chronic renal failure, the filtration function suffers to varying degrees and breakdown products (uremic toxins) are not excreted from the body. The criteria for chronic renal failure are: blood urea and creatinine concentrations.
Creatinine is the end product of protein metabolism, which breaks down during muscle contractions. This is an important indicator of kidney function because creatinine is excreted in the urine. Urea is a nitrogen-containing breakdown product of proteins and, in general, its production is proportional to protein consumption: from 100 g of protein consumed, 30 g of urea is formed. In patients with chronic renal failure, it is possible to delay the period of increase in urea in the blood by reducing protein intake to 20–30 g per day.
In this regard, patients with renal failure are advised to eat a protein-restricted diet. The patient can consume such an amount of protein that will not cause an increase in azotemia . By limiting protein intake, the level of urea decreases, and the symptoms of uremic intoxication (nausea, vomiting, uremic gastritis, colitis, itching) disappear.
Diet can slow the progression of the disease and prolong the life of patients. The first stage of kidney damage is hyperfiltration (increased filtration), which is associated with an increase in the load on the glomeruli of the kidneys. Hyperfiltration is one of the mechanisms of progression of renal failure. Reducing the protein load inhibits it and, therefore, slows down the progression of the disease.
General nutrition rules:
- The main thing is to limit the consumption of animal protein.
- Reduce phosphorus-containing foods, salt and liquid. All dishes are prepared without salt and its consumption is allowed in the amount of 1.5–2.5 g per day in ready-made dishes.
- Fractional diet.
- Monitor potassium and magnesium intake.
- Increased energy value of the diet - at least 3000-3500 kcal due to fats and carbohydrates.
- Increase in unsaturated fatty acids (vegetable oils and nuts, if there are no restrictions on potassium and phosphorus).
- Adequate intake of vitamins.
- Culinary processing - baking, boiling, frying without a pronounced crust.
- Limit or eliminate nitrogenous extractives, strong coffee, alcohol, chocolate, tea, cocoa and salty snacks.
Patients can be prescribed Diets No. 7 , 7A , 7B , which differ in protein composition. In the initial stage of the disease, a protein content of 0.8 g/kg of weight is allowed. Regular bread is replaced with protein-free bread. The patient is recommended to have fasting days with a reduced amount of protein three times a week. Patients at this stage do not need additional intake of amino acid
For stage 2 chronic renal failure, protein is limited to 0.5-0.4 g/kg body weight. Due to the recommended phosphorus restriction, the patient should not consume legumes, poultry, egg yolks, nuts, cheeses, and milk in limited quantities.
To reduce phosphates in beef, rice, fish or potatoes, boil them several times, constantly draining the water. Due to the restriction of animal protein, amino acid supplements are prescribed (drug Ketosteril ). In addition to the fact that the drug is a supplier of essential amino acids, the calcium contained in it binds phosphates and is removed from the intestines.
The prescription of a diet containing 0.3 g of protein per kg of weight is indicated for stage 3 chronic renal failure.
In parallel, preparations of essential amino acids . The diet of patients includes foods with a small amount of protein, but high in calories - sago, protein-free bread, mashed potatoes with corn starch.
In case of disturbances in the electrolyte composition of the blood, limit the consumption of potassium (dried apricots, apricots, raisins, prunes, potatoes), magnesium (cereals, legumes, bran, fish, cottage cheese) and phosphates (cheeses and dairy products). In conditions of reduced protein intake in patients, it is necessary to maintain nitrogen balance.
Thanks to the variety and availability of foods with dosed protein content, the diet has become easy and not burdensome to follow. The dry mixture “Diso” “Nutrinor” contains 40 g of high-value protein per 100 g. The mixture in an amount of 9-28 g is introduced into a dish 3 minutes before readiness, for example, into porridge, soup or vegetable dishes.
When is a protein-free diet necessary?
To use such a power supply scheme, the following reasons are required:
- oncological diseases;
- pathologies of brain lymphoid tissue;
- kidney and liver diseases.
In the presence of the listed diagnoses, a special diet is required, excluding heavy foods, fatty, fried foods, marinades, canned food, and pickles. The basic list of foods on a protein-free diet consists of fresh, boiled vegetables, whole grain cereals and vegetable fats.
Reducing proteins in the menu is justified from a medical point of view. Limiting or completely avoiding foods high in this substance reduces the load on the lymphatic system. At this time, previously accumulated reserves are actively used up. As a result, the body is cleansed of waste and toxins, and immunity increases.
Authorized Products
A low protein diet involves eating:
- Protein-free bread made from corn starch up to 300 g per day. This bread is also salt-free.
- Vegetarian cereal and vegetable soups in the amount of 250 ml per serving.
- Lean beef, chicken, turkey, boiled, as well as baked or fried after boiling, which removes nitrogenous substances. Average portion of meat 60 g.
- Low-fat fish - preparation methods and portions are the same.
- Vegetables - carrots, dill, cucumbers, cauliflower, green onions, lettuce, parsley, potatoes, cabbage. If a low-potassium diet is indicated for the patient, the vegetables are soaked, then boiled, draining the water several times, after which they can be stewed or baked.
- Cereals, legumes and pasta in limited quantities due to the content of protein, potassium and phosphorus. Sago dishes are recommended. Regular grains need to be soaked before cooking. Pasta and rice contain less potassium than potatoes.
- One egg white omelet.
- Berries and fruits in natural form and boiled. If it is necessary to limit potassium, fruits with a high potassium content (oranges, tangerines, bananas, dried apricots, raisins, figs) are sharply limited or excluded from the diet. The potassium content decreases slightly when fruit is boiled.
- Milk and fermented milk products, unless there are restrictions on phosphorus and protein. They can be consumed 200-300 g per day. You can consume cottage cheese in small quantities (up to 50 g), unless your doctor prescribes its exclusion.
- Weak tea, herbal teas, rosehip infusion. The possibility of drinking fruit juices due to the presence of potassium in them is discussed with your doctor.
- Unsalted butter and vegetable oils.
- Dishes are prepared without salt.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| green onion | 1,3 | 0,0 | 4,6 | 19 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| beet | 1,5 | 0,1 | 8,8 | 40 |
| celery | 0,9 | 0,1 | 2,1 | 12 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| garlic | 6,5 | 0,5 | 29,9 | 143 |
Fruits | ||||
| watermelon | 0,6 | 0,1 | 5,8 | 25 |
| melon | 0,6 | 0,3 | 7,4 | 33 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Berries | ||||
| strawberry | 0,8 | 0,4 | 7,5 | 41 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
| sago | 1,0 | 0,7 | 85,0 | 350 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jelly | 2,7 | 0,0 | 17,9 | 79 |
| milk candies | 2,7 | 4,3 | 82,3 | 364 |
| fondant candies | 2,2 | 4,6 | 83,6 | 369 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| cinnamon | 3,9 | 3,2 | 79,8 | 261 |
| honey | 0,8 | 0,0 | 81,5 | 329 |
| ground black pepper | 10,4 | 3,3 | 38,7 | 251 |
| dried parsley | 22,4 | 4,4 | 21,2 | 276 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
| milk sauce | 2,0 | 7,1 | 5,2 | 84 |
| sour cream sauce | 1,9 | 5,7 | 5,2 | 78 |
| caraway | 19,8 | 14,6 | 11,9 | 333 |
| dried dill | 2,5 | 0,5 | 6,3 | 40 |
Dairy | ||||
| milk | 3,2 | 3,6 | 4,8 | 64 |
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| cream | 2,8 | 20,0 | 3,7 | 205 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| curdled milk | 2,9 | 2,5 | 4,1 | 53 |
| acidophilus | 2,8 | 3,2 | 3,8 | 57 |
| yogurt | 4,3 | 2,0 | 6,2 | 60 |
Meat products | ||||
| boiled beef | 25,8 | 16,8 | 0,0 | 254 |
| boiled beef tongue | 23,9 | 15,0 | 0,0 | 231 |
| boiled veal | 30,7 | 0,9 | 0,0 | 131 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken | 25,2 | 7,4 | 0,0 | 170 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Oils and fats | ||||
| corn oil | 0,0 | 99,9 | 0,0 | 899 |
| olive oil | 0,0 | 99,8 | 0,0 | 898 |
| sunflower oil | 0,0 | 99,9 | 0,0 | 899 |
| ghee | 0,2 | 99,0 | 0,0 | 892 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| black tea with milk and sugar | 0,7 | 0,8 | 8,2 | 43 |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| * data is per 100 g of product | ||||
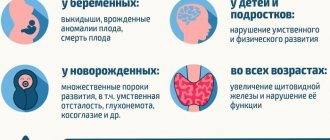
Treatment of phenylketonuria
Currently, drugs are being developed that will allow you to control the level of phenylalanine in the blood without following a diet. There has been significant progress in this direction, but such medicines will not appear on sale earlier than in 5–7 years. Work is constantly underway to find new means and methods of combating the disease:
1. A promising direction is the use of the plant enzyme phenylalanine lyase, which will break down excess phenylalanine in the body.
2. Scientists have high hopes for gene therapy using a viral factor, which will cure the diseased gene and completely get rid of the problem.
3. It is practiced to introduce the phenylalanine hydroxylase gene directly into the affected liver cells.
But in our country these developments are not yet used. Today in Russia the only effective method of treating phenylketonuria is diet therapy.
Treatment with diet is the main help for patients with phenylketonuria. From birth until puberty, they need to limit their protein intake. The growth and development of the child should be constantly monitored by doctors: a pediatrician and a neurologist. Medical genetic consultation specialists and nutritionists must adjust the amount of proteins so that it corresponds to the age and load of the child.
Some forms of phenylketonuria can be treated with tetrahydrobiopterin, which is a component of the missing enzyme phenylalanine 4-hydroxylase. Atypical forms of phenylketonuria cannot be treated with diet and require regular intake of tetrahydrobiopterin or its substitutes.
Table 2. Age norms for phenylalanine
| Child's age | Daily amount of phenylalanine (mg/kg body weight) |
| Up to 2 months | 60 |
| 2–3 months | 60–55 |
| 3–6 months | 55–45 |
| 6–12 months | 45–35 |
| 1–1.5 years | 35–30 |
| 1.5–3 years | 30–25 |
| 3–6 years | 25–15 |
| Over 6 years old | 15–10 |
Nutrition of a patient with phenylketonuria
Comprehensive information about the optimal composition of specialized medicinal products for patients with phenylketonuria of various age groups and dietary therapy tactics using these products is presented in the methodological letter “Specialized medicinal products for nutrition of children with phenylketonuria” (Moscow, 2012), prepared by specialists from the Federal State Budgetary Institution “Research Center for Health” children", Federal State Budgetary Institution "Research Institute of Nutrition", Federal State Budgetary Institution "Moscow Research Institute of Pediatrics and Pediatric Surgery".
In accordance with the recommendations of the methodological letter, when organizing diet therapy for a patient with phenylketonuria, it is important to completely exclude animal proteins from the diet so that the child’s nerve cells are not exposed to the toxic effects of phenylalanine and its derivatives. If this is done in the first weeks of life, the brain will remain completely healthy. If you start limiting protein at a later age, then the developmental delay can be somewhat stopped. But it will no longer be possible to restore health to the nervous system and eliminate changes in nerve cells.
All amino acids necessary for growth and development are supplied to the body from specialized medicinal products. They usually come in the form of a powder - a dry mixture of amino acids. Parents of a sick child are given these products free of charge during a medical genetic consultation. Infants receive special formulas, completely free of lactose, based on milk protein hydrolyzate.
Nutrients that should replace natural protein products for children contain:
- peptides (milk proteins digested by enzymes);
- free amino acids (tyrosine, tryptophan, cystine, histidine and taurine).
Currently in Russia, various specialized products of domestic and foreign production are used based on mixtures of amino acids without phenylalanine: “Aphenilak 0–12”, “Aphenilak”, “Tetrafen 40”, “Tetrafen 70” (Nutritek, Russia), “Analog” -XP (Nutritsia, Holland), MDmil PKU-0, MDmil PKU-1 (Hero, Spain), Phenyl Free 1, Phenyl Free 2 (Mead Johnson, USA). The products are powders that must be diluted with boiled water or expressed breast milk, according to the instructions. The result is a liquid mixture or “sour cream.” This complementary feeding is introduced gradually over 2–5 days under the supervision of a doctor. Children with phenylketonuria can be breastfed. But at the same time, a nursing mother needs to adhere to a special diet.
In the diet of preschool and school-age children, protein products are completely excluded from the menu. The list of permitted products includes vegetables, fruits, starch products, and vegetable oils. When compiling a daily menu, it is necessary to strictly adhere to the age standards for phenylalanine. However, it is necessary to take into account the patient’s individual tolerance to phenylalanine, which is determined during the treatment process.
It must be remembered that nutritious nutrition is vital for a growing body. So, a child needs 120 mg of tyrosine per kilogram of weight per day. Therefore, children and adolescents with this diagnosis must receive amino acids for cell building and growth from additional sources. A vitamin-mineral complex is also required. It is especially important that the child receives the norm of vitamins C, B6 and B1, folic acid, iron, calcium and magnesium.
Food traffic light
In most countries, natural products on which the diet is based are divided into three groups based on their protein content, which make up the so-called food traffic light of a patient with phenylketonuria (see Fig. 1).
Rice. 1. “Food traffic light” of a patient with phenylketonuria
The industry produces two more groups of products:
- artificial low-protein products, especially for dietary nutrition (bread, cookies, pasta) - loprofines;
- ready-made fruit-based purees for baby food.
The red list includes foods high in phenylalanine, which are completely excluded from the diet of patients with PKU.
Orange list - products that contain moderate amounts of protein and therefore phenylalanine and should therefore be used with caution in small quantities and under systematic monitoring of blood phenylalanine. They should also be distributed evenly throughout the day.
Green List - products containing trace amounts of phenylalanine, which can be used completely freely in normal quantities.
Nutrition of children of the first year of life
To organize dietary nutrition for children in the first year of life, the Union of Pediatricians of Russia, together with the Federal State Budgetary Institution "Scientific Center for Children's Health", the Federal State Budgetary Institution "Research Institute of Nutrition", departments of pediatrics of medical universities and academies, developed a scientific and practical program "National Strategy for Feeding Children of the First Year of Life in the Russian Federation" . The program provides modern science-based approaches to optimizing the nutrition of healthy and sick infants, as well as pregnant women and nursing mothers.
In accordance with the developed program, the first thing to begin with in prescribing diet therapy for children of the first year of life with the disease “phenylketonuria” is the daily content of phenylalanine (an essential amino acid) in the diet of the sick child. High levels of phenylalanine in the blood are detrimental to brain development, while insufficient levels of this essential amino acid can cause a negative nitrogen balance. To date, the limiting concentration of phenylalanine in the blood at which brain damage occurs has not been determined, so it is necessary to determine the individual tolerance to phenylalanine in each child.
Equivalent replacement for protein and phenylalanine is made using the “portion” calculation method: 50 mg of phenylalanine is approximately equivalent to 1 g of protein, which allows for adequate replacement of products for protein and phenylalanine. Since phenylalanine is an essential amino acid, the minimum requirement for it must be met to ensure normal growth and development of a child with phenylketonuria. The smaller the child, the more phenylalanine he needs, since, unlike adults, 40% of dietary phenylalanine in children is spent on the synthesis of the body’s own proteins.
Specialized products based on a mixture of amino acids are introduced into the diet gradually, over 10–14 days, the initial doses are 1/5–1/10 of their required daily amount. At the same time, the proportion of protein from natural products in the diet is reduced, and a specialized product is added to each meal. In the first months of life, the only source of protein from natural products is expressed human milk or infant formula, the protein content of which should not exceed 10–12 g per 100 g of dry formula. Expressed human milk or formula is combined with the required amount of a specialized product, diluted with boiled water or special water for baby food, while the total amount of food corresponds to the patient’s age. It is recommended to prepare food before each feeding.
Other approaches to prescribing a diet for an infant are also possible. If the level of phenylalanine in the blood is very high (900–1200 mmol/l), when switching to a therapeutic diet, it is recommended to feed the patient for 2–3 days only a specialized product based on a mixture of amino acids without phenylalanine or a protein hydrolyzate with a low content. This allows you to more intensively reduce the level of phenylalanine in the blood. After its normalization, expressed human milk or infant formula is gradually included in the diet. When switching to an elemental diet, the amount of medicinal mixture and products with natural protein (women's milk or baby formula, later complementary foods) is calculated. The chemical composition of the diet is calculated in accordance with the age needs of the child.
Table 3. Features of the composition and timing of introduction of complementary feeding products
| Products and dishes | Timing of introduction of complementary foods (months) | |
| Children with PKU | Healthy children | |
| Fruit juice | 3 | 3 |
| Fruit puree | 3,5 | 3,5 |
| Vegetable puree | 4–4,5 | 4,5 |
| Protein-free porridge | 5 | – |
| Protein-free jelly | 6 | – |
| Protein-free vermicelli | 7 | – |
| Protein-free bread | 8 | – |
| Milk porridge | – | 5 |
| Cottage cheese | – | 5 |
| Egg | – | 6 |
| Meat | – | 7 |
| Kefir | – | 7 |
| Rusks, cookies | – | 6 |
| Vegetable oil | 4 | 4 |
| Butter | 5 | 5 |
Purpose of complementary feeding
From 3 months of age, the diet of a patient with phenylketonuria is expanded to include fruit and berry juices (apple, pear, plum, etc.), starting with 5–10 drops, gradually increasing the volume, bringing it to 30–50 ml/day, by the end of the year - up to 100 ml.
From 3.5 months, fruit puree is prescribed, the amount of which is increased in the same way as when introducing juice.
From 4–4.5 months, the first complementary foods are introduced into the diet in the form of vegetable puree or canned fruits and vegetables for baby food without the addition of milk.
At 5 months, a second complementary feeding is prescribed - 10% porridge made from ground sago or protein-free grains. Industrially produced dairy-free porridges based on corn and rice flour, containing no more than 1.0 g of protein per 100 ml of ready-to-eat food, can also be used as complementary foods.
From 6–7 months, mousses and jelly are introduced into the diet, which are prepared using amylopectin swelling starch and fruit juice. Features of the composition of complementary feeding products, as well as the timing of their introduction, are reflected in Table 3.
Fully or partially limited products
- Broths (fish, meat and mushroom).
- Animal fats.
- Salty products: canned food, cheeses, chips, sausages, sauces, ketchups, salted nuts, marinades, soup concentrates, bouillon cubes, margarine, salted butter.
- Potassium-containing foods: sorrel, bananas, coffee, milk powder, millet porridge, curry, fruit juices, fish, meat, chocolate, rhubarb, avocado, seeds, sesame, dried fruits, potatoes, many nuts (primarily almonds, peanuts, pine nuts) , peanut butter and paste, wine, beer, parsley, tomatoes (and products made from them - ketchup, sauce, juice), spinach, apple juice and syrup, beets, artichokes, soy products, soybeans, mushrooms, beans, lentils.
- Phosphorus-containing products: milk, cheeses, liver, kidneys, fish, fish caviar, chocolate, mushrooms, bran, nuts, seeds.
- Alcohol and carbonated drinks.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| sauerkraut | 1,8 | 0,1 | 4,4 | 19 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| canned cucumbers | 2,8 | 0,0 | 1,3 | 16 |
| pickles | 0,8 | 0,1 | 1,7 | 11 |
| radish | 1,2 | 0,1 | 3,4 | 19 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| turnip | 1,5 | 0,1 | 6,2 | 30 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| canned tomatoes | 1,1 | 0,1 | 3,5 | 20 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Fruits | ||||
| apricots | 0,9 | 0,1 | 10,8 | 41 |
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| figs | 0,7 | 0,2 | 13,7 | 49 |
| nectarine | 0,9 | 0,2 | 11,8 | 48 |
| peaches | 0,9 | 0,1 | 11,3 | 46 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
| marinated mushrooms | 2,2 | 0,4 | 0,0 | 20 |
Nuts and dried fruits | ||||
| raisin | 2,9 | 0,6 | 66,0 | 264 |
| dried apricots | 5,2 | 0,3 | 51,0 | 215 |
| dried apricots | 5,0 | 0,4 | 50,6 | 213 |
| dates | 2,5 | 0,5 | 69,2 | 274 |
Cereals and porridges | ||||
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| ginger | 1,8 | 0,8 | 15,8 | 80 |
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
| tomato sauce | 1,7 | 7,8 | 4,5 | 80 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| salmon caviar granular | 32,0 | 15,0 | 0,0 | 263 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Juices and compotes | ||||
| tomato juice | 1,1 | 0,2 | 3,8 | 21 |
| * data is per 100 g of product | ||||
Basic rules of a protein-free diet
Completely eliminating protein from the diet is prohibited. According to WHO, an adult needs 0.75 g of the substance per kilogram of weight. In case of kidney disease, the norm decreases to 0.55 g.
The key principles of the low protein system include the following:
- Minimum use or complete exclusion of salt and hot spices from the diet.
- Reducing water consumption to 0.8-1 liters per day. It is better to use bottled water without gas.
- Acceptable methods of heat treatment of food are boiling, stewing, steaming, baking. Using frying or smoking is unacceptable.
- Eat small portions - 250-300 g. During the day there should be 4-6 meals. Dinner is allowed no later than 2-3 hours before bedtime.
Strength training and vigorous physical activity will also have to be postponed. Limited protein intake leads to gradual breakdown of muscle tissue. The body begins to use muscle structures to provide the necessary energy to all vital systems.
Be sure to read: LCHF diet: allowed and prohibited foods, weekly menu by day and recipes
Menu (Power Mode)
Strict compliance with the requirements and calculation of the amount of protein, potassium and phosphorus makes it possible to improve the patient’s quality of life and extend the dialysis-free period. For calculations, patients use tables of protein, phosphorus and potassium content in foods.
Six grams of animal protein are contained in: one egg, 30 g of fish, 25 g of meat, 60 g of sour cream, 25 g of cheese, 150 g of yogurt and 25 g of seafood. Two grams of vegetable protein contain 120 g of potatoes, 150 g of oatmeal and 100 g of rice. To add flavor to food, you can use small amounts of dill, bay leaf, parsley, basil, cinnamon, onion, cloves or garlic. You can use low-protein products: amylopectin starch, sago, bread made from maize starch.
It is impossible to create a universal menu suitable for all patients, since the degree of azotemia and disturbances in phosphorus-potassium metabolism are different for everyone. When drawing up a menu, you need to base it on the doctor’s recommendation. An approximate menu for Table 7B might look like this:
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Protein-free diet: weight loss results
Anna, 27 years old
“I tried low carb for about 10 days. It was not easy, but I managed to endure it. I practically didn’t eat meat, eggs, white bread or pasta. True, I couldn’t completely give up salt; I added a little to porridge and soups. I was able to lose 3.5 kilograms, but the weight began to return again. So the game wasn’t worth the candle.”
Elena Petrovna, 44 years old
“I followed a special diet for a week on the doctor’s recommendation. I have acute renal failure, I can’t do it without diet. They said you need to avoid consuming foods that contain a lot of potassium - bananas, nuts, broccoli. I ate porridge, boiled vegetables (potatoes, carrots, zucchini), cornmeal bread and some fish. I excluded everything salty and fatty. I even had to buy a double boiler, and now I cook everything only in it. I felt lighter and began to swell less. I want to repeat the course in six months.”
Christina, 21 years old
“Diets are a sore subject for me, I’m always trying to lose weight. I chose this one because I eat little meat and don’t like cottage cheese or cheese. But I was only able to eat like this for 5 days; food without salt turned out to be very tasteless. I didn’t want to cook anything; I ate almost nothing but raw vegetables and fruits. In recent days, my stomach has been very sick, my stool has become irregular, and I have become irritable. To my surprise, I lost 1.5 kg. But I don't plan to continue. I will look for other options."
Artemy, 39 years old
“A low-protein diet without salt is very difficult to tolerate. Even seasonings don’t help me; the food seems absolutely tasteless. But this is how my doctor prescribed me to eat. Any canned food, marinades, fried potatoes, or store-bought semi-finished products are prohibited. Now my wife cooks for me separately, steaming everything. I’ve been following the regime for 7 days now, there’s not much left. But I feel better, that’s why I’m holding on.”
Low protein diet recipes for kidney disease
In the initial form of chronic renal failure, the method of cooking does not matter - frying, boiling and baking are allowed. In case of severe renal failure, when it is necessary to limit potassium, the products must first be boiled. Thus, its content is reduced by almost half (the microelement passes into water).
Potatoes, beets, eggplants and zucchini are rich in potassium, so they are peeled and pre-boiled. In the future, use it at your own discretion. Those suffering from kidney failure can use seasonings and spices - pepper, vinegar, mustard, herbs.
Compote must be prepared from apples and pears; it is not allowed to add dried apricots and raisins to the decoctions due to the high potassium content. In the non-dialysis period for stage 2 chronic renal failure, a diet with 0.6 g/kg of protein is recommended, half of which should be animal proteins. The usual serving of meat or fish is 50 g per day.
Patients can use sago cereal - it contains only 1 g of protein, has no taste and absorbs the flavors of other foods well. It can be combined with rice, herbs and spices, meat products and vegetables. The sago is soaked overnight and boiled for 30-40 minutes in the morning. After this, discard in a colander, rinse and lightly dry. The finished porridge can be stored in the refrigerator and used as needed.
First meal
Vegetarian borscht
Boil the peeled beets until half cooked, remove and grate them. Stew onion, tomato and grated carrots in vegetable oil. Dip the prepared potatoes (soaked) into the beet broth. Boil for 15 minutes and add the chopped cabbage, and after 3 minutes add the stewed vegetables. Season the dish with herbs and sour cream.
Second courses
Sago and rice milk porridge
Take equal quantities of rice and sago, previously soaked. Pour water in a ratio of 1:2 and put on fire. Cook over low heat for about 45 minutes. Add a glass of milk, sugar to the finished porridge and bring to a boil. Serve with butter.
Sago with meat
Prepare a portion of sago or use pre-prepared porridge. Heat it in a water bath. Separately, cook the beef, draining the water. Take 50 g of meat per serving, you can mince it, lightly fry it with onions and mix the resulting minced meat with sago.
Potato zrazy with cabbage
Peel the potatoes, cut into pieces and soak for an hour. Boil, cool and grind thoroughly (you can use a meat grinder). Separately, stew the white cabbage, adding bay leaf, pepper and dill. Make a flat cake from the potato mixture, put minced cabbage on it and seal the edges, giving the zrazas the shape of a pie. Fry in vegetable oil. Can be served with sour cream.
Dessert
Carrot cutlets
Peel and boil the carrots. Grate the cooled mixture on a fine grater. Add sugar, 2 tbsp. l. semolina, mix well and let stand for the cereal to swell. Make cutlets from the resulting mass. Fry in vegetable oil on both sides until browned. Serve with sour cream.
Rules for protein-free nutrition
In order for the desired effect to occur much faster, the following recommendations should be followed.
The daily menu should contain:
- carbohydrates - three hundred and fifty grams;
- fat - eighty grams;
- plant foods - one fourth of the total diet;
- protein - permissible norm - twenty grams;
- salt - no more than two grams.
Dishes containing any sauces or hot seasonings are excluded from the menu.
During the diet - refusal of active physical activity, strict adherence to the diet and diet.
Sticking to a protein-free diet for a long time can harm your health.
Reviews and results
This diet is not easy to follow because it has many restrictions and takes into account many nutritional factors. But such nutrition is a vital necessity for patients. Strict control of potassium and phosphorus adds further restrictions. However, patients have adapted to such a dietary diet, supplement it with protein-free foods and amino acid , and consider unsalted and tasteless dishes to be the only drawback.
- “... High blood pressure and creatinine forced me to make adjustments to my diet. Only diet helps. At this stage, I sharply limited the salt, removed cottage cheese and cheese, I don’t eat fish - I don’t like it. I limited my meat a little (at the expense of pork and beef, I’m generally indifferent to meat). Main food: potatoes, rice, cabbage, zucchini, rolled oats, butter and vegetable oil, I drink milk, but not every day. I really love vegetables in any form (cutlets, casseroles, stews, purees) and they help me out. The course of chronic renal failure will make adjustments and it will be clear what to do next”;
- “... I’ve already adapted to this diet. For breakfast - rolled oats with water, add honey, a little apple, I can make an omelet or milk rice porridge or sago. I buy homemade unleavened cheese (like Adyghe cheese) and tea. For lunch I cook boiled meat or bake it. As a side dish I use rice, buckwheat, stewed cabbage or zucchini. I add pepper, onion, garlic, and basil to all dishes. For now, I don’t limit vegetables and fruits, except for the leaders in potassium (bananas, dried apricots, dates, raisins). I go on business trips and even there I solve the nutrition problem: I take food in containers (rice and boiled chicken/turkey). Of course, I want meat, but I can’t have too much, so I add just a spoonful of minced meat to the porridge. I can only eat 50 g of meat per day. I don’t count anything other than protein. It's good that low-protein foods exist and this allows you to eat better and follow a diet. I buy protein-free flour and bake my own bread, cereals, pasta, and cookies. Pasta tastes no different from regular pasta. I use scales that calculate the content of foods based on protein, salt, fats, carbohydrates, and show calories. Potassium, if necessary, can be taken from the tables. Thus, for health reasons I have been at the same level for 4 years already”;
- “... Nutrition for chronic renal failure is very important. Previously, I only limited protein, but now the potassium level has increased, and the doctor said to be sure to take this into account. Therefore, I excluded tomatoes, peppers, chocolate, bananas, dried fruits, citrus fruits - I can only add a slice of lemon, a slice of orange or tangerine to tea. I eat eggplants, but I soak them in salt water for 30 minutes, they release juice and lose microelements. Then I fill it with fresh water, soak it and squeeze it out. I do the same with cabbage. I eat unsalted, several times boiled rice with zucchini or nori. For taste, I sprinkle with turmeric, green onions and sunflower oil. I also eat buckwheat and corn porridge - there is more protein than in rice, but there is less phosphorus. I mix calcium carbonate with food and drink Ketosteril 12 tablets a day. He doesn’t make me want to eat.”
Protein-free diet: list of products
In its strict form, a protein-free diet excludes almost all components of animal origin, replacing them with mixtures and essences containing the necessary complex of amino acids.
Most nutritionists create a more gentle and balanced version of the diet, where some animal proteins are present.
Authorized Products
| № | Name | Scroll |
| 1 | Bakery products | Bran, white protein-free bread, cereal flakes, crispbread |
| 2 | Meat fish | Lean turkey, rabbit, hake, pollock, pike |
| 3 | Egg | One a day |
| 4 | Vegetables | Almost all |
| 5 | Cereals | Any pasta other than regular legumes (peas, chickpeas) |
| 6 | Fruits | Everything except melon and watermelon |
| 7 | Oils | Vegetable, flaxseed, olive |
| 8 | Milk | Low-fat milk, kefir |
| 9 | Beverages | Tea, coffee (in limited quantities), compotes, jelly, herbal and berry infusions |
| 10 | Sweet | Honey, preserves, jams, jellies |
Prohibited Products
| № | Name | List |
| 1 | Animal fats | Butter, ghee, margarine, lard |
| 2 | Meat | Chicken, beef, pork |
| 3 | Milk | Full-fat sour cream, cottage cheese, cheese, cream |
| 4 | Bakery products, sweets | Baked goods, shortbread, biscuits, sweets, cakes, regular bread |
| 5 | Vegetables | Radish, daikon, radish, garlic, horseradish, pumpkin, hot pepper |
| 6 | Beverages | Soda, alcohol |
| 7 | Other | Marinades, canned food, mushrooms, soy, nuts, seeds, chips, smoked meats |