The role of testosterone in the male body
Testosterone, like some other hormones, is produced in the testicles, that is, in the male testicles.
The processes of so-called virilization, that is, the development of secondary and tertiary male sexual characteristics, depend on the testosterone content in the male body:
- Formation of appearance, including the skeleton, face and facial expressions according to the male type.
- Sizes of genital organs and their function.
- Prostate secretion production.
- Physical strength and endurance.
- Voice timbre (with normal testosterone levels, a man has a low or rough voice).
- Density of hair, growth of mustache, beard.
- Intensity and sharpness of the odor.
- Increase in muscle mass and its distribution “according to the male type”.
- Mental and emotional state: attentiveness, speed of reaction, adequacy of behavior, reaction to danger.
Treatment of hypogonadism in men
When starting to treat hypogonadism, the doctor sets a number of goals:
- elimination of androgen deficiency (restoration of potency, libido, well-being and behavior);
- ensuring virilization (growth of hair on the face and body according to the male type, change in voice timbre, physique, increase in muscle mass, enlargement of the penis and testicles, pigmentation of the scrotum, development of folding), if possible, ensuring fertility;
- potentially - reducing cardiovascular risks, preventing osteoporosis.
Depending on whether it is necessary to restore fertility, the choice of therapy is between hormone replacement therapy (HRT) with testosterone preparations, on the one hand, and preparations of human chorionic gonadotropin (hCG), luteinizing hormone (LH), follicle-stimulating hormone (FSH) and gonadotropin- releasing hormone (GRH) - on the other.
There are a large number of dosage forms of testosterone for intramuscular, subcutaneous, transdermal, oral and buccal use. However, testosterone HRT leads to a decrease in testicular volume and suppression of spermatogenesis.
Therefore, if testicular function is preserved and hypogonadism is of hypothalamic or pituitary origin, either hCG, LH, FSH drugs, or pulsatory administration of GnRH are used. These hormones increase the production of your own testosterone, which leads to the induction of spermatogenesis and restoration of fertility.
Clinical case
Patient K. (39 years old) consulted an endocrinologist with complaints of sexual dysfunction (decreased sexual desire, erectile dysfunction), general weakness, increased fatigue, shortness of breath during exercise, episodes of increased blood pressure (maximum up to 165/100 mm Hg). .), excess weight, ineffectiveness of physical activity and diets.
He said that he follows the principles of rational nutrition and regularly visits the gym. The above complaints have been bothering me for the last year. He was not independently treated or examined. Objectively upon examination:
- height - 183 cm;
- weight - 127 kg;
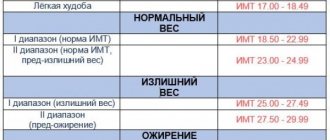
- BMI - 37.9 kg/m2;
- waist circumference (WC) - 123 cm;
- hip circumference (HC) - 135 cm;
- OT/OB - 0.91;
- Blood pressure - 145/90 mm Hg. Art., heart rate - 82 beats per minute.
Hair growth in the armpits, chest, anterior abdominal wall, and groin area is unremarkable. Bilateral false gynecomastia. The external genitalia are formed correctly, without any peculiarities.
When using the ADAM questionnaire, positive answers to 8 out of 10 questions, which indicates the severity of symptoms of androgen deficiency in this patient.
Laboratory indicators:
- total cholesterol - 6.4 mmol/l (normal 3.1–5.2);
- LDL - 3.8 mmol/l (normal 0–3.3);
- triglycerides - 2.6 mmol/l (normal - less than 2.3);
- total testosterone - 7.2 nmol/l (normal 12.0–41.0);
- SSSH - 28.9 pmol/l (normal 12.9–61.7);
- LH - 4.7 U/l (normal 2.5–11.0);
- TSH - 1.8 mU/l (normal 0.25–4.0);
- prolactin - 243 IU/l (normal 50–610);
- estradiol - 164 pmol/l (normal 20–240);
- total PSA - 0.6 ng/ml (normal 0-4).
According to ultrasound of the prostate gland, no echographic signs of pathology were identified.
The patient was diagnosed with normogonadotropic hypogonadism.
Metabolic syndrome: Abdominal obesity (2nd degree). Arterial hypertension. Dyslipidemia. Treatment goals:
Normalization of testosterone levels. A prolonged form of testosterone (testosterone undecanoate 1000 mg) was prescribed intramuscularly according to a regimen with dose titration to maintenance.
Weight loss and maintenance. It is recommended to follow the principles of a balanced diet with limited consumption of fats and easily digestible carbohydrates, table salt, as well as additional aerobic exercise (active walking for 1 hour a day).
When assessing the results of therapy after 10 months, the patient noted significant positive dynamics in general well-being - improvement in erectile function (increased sexual desire, increased frequency of spontaneous erections), disappearance of complaints about fatigue, depressed mood; stabilization of blood pressure to 130/80 mm Hg. Art. Objectively, upon examination, there was a decrease in all anthropometric indicators: weight - 99 kg, BMI - 29.5 kg/m2, WC - 88 cm, WC - 109 cm, WC/WC - 0.81. During treatment, all hormonal and biochemical parameters also normalized. In the future, it was decided to continue therapy with monitoring of laboratory parameters once every six months.
Testosterone norm
The normal testosterone level in a healthy man is 12-33 n/mol. Testosterone levels in the blood can fluctuate throughout the day. For example, the level increases when playing sports or before sexual intercourse. In addition, different laboratories use different methods to determine testosterone concentrations, so the test form usually states the normal testosterone value for that laboratory.
If testosterone levels are below normal, this can lead to the following consequences:
- Decreased libido.
- Testicular dystrophy and other pathological processes.
- Problems with erection and conception.
- Disturbance of sexual development.
- Pathologies of the pituitary gland or hypothalamus.
Signs of Low Testosterone
The following signs may indicate insufficient testosterone levels in a man:
- Lack or decreased sexual desire.
- Decreased quantity and quality of erections.
- Reducing the duration of sexual intercourse.
- Depression, irritability, loss of interest in the world around you.
- Physical weakness.
- Memory impairment, absent-mindedness, impaired cognitive function.
- Frequent urination with a weak stream.
- Sleep disturbance, constant feeling of fatigue.
With age, testosterone levels naturally decrease as the testes, hypothalamus and pituitary gland, which are responsible for the secretion and activation of the hormone, age. At the same time, this process occurs quite slowly. However, if signs of low testosterone appear before the age of 50, it is recommended to consult an andrologist. It is recommended to regularly check hormone levels from the age of 40 in order to take the necessary measures in time.
What is testosterone
This is a hormone with a pronounced anabolic effect, which is produced in men both in the adrenal glands and in the testicles. Moreover, more of it is synthesized in the gonads, and its high concentration is created there.
How is testosterone produced in men? It is formed by special testicular cells from cholesterol and is a prohormone in its structure. To produce all of the above effects, testosterone must be processed by the enzyme 5-alpha reductase. This produces the active form of testosterone, dihydrotestosterone.
The luteinizing hormone of the pituitary gland (LH) gives the “command” to the production of testosterone. If testosterone levels decrease, a signal is sent to the pituitary gland to produce more LH and therefore testosterone. If a man’s testosterone level is elevated (for example, he takes synthetic drugs), then LH decreases. And when a man stops taking his supplements, it may take a long time before LH levels return to normal and give the “command” to synthesize his own testosterone.
What determines testosterone levels in men?
A complex of factors is important for the synthesis of this hormone:
- male physical activity;
- nature of nutrition: content of cholesterol and vitamin D in food;
- condition of testicular cells: they can be damaged reversibly (with bacterial orchitis, which was cured in time) or irreversibly (for example, with mumps - mumps, with diabetes, severe testicular trauma, varicocele);
- a condition of the pituitary gland in which LH is produced;
- medications taken (for example, anticancer drugs inhibit the activity of testicular cells);
- the level of estrogen in the male body: when it decreases, the amount of testosterone also decreases;
- prolactin level (high levels of this hormone reduce testosterone synthesis).
How to determine testosterone levels
To determine the content of androgen hormones, which include testosterone, venous blood is donated. To determine a man's testosterone level, a urine test is also taken. Blood is taken in the morning, since this is the time when testosterone levels are most adequate and comparable to general well-being. In some cases, a bone tissue examination is prescribed. This is explained by the fact that low testosterone levels in men can cause osteopathy.
After receiving the test results, if necessary, appropriate therapy is prescribed to increase testosterone. In this case, the doctor chooses methods and means that will affect not only the level of testosterone itself, but also the reasons that led to insufficient levels of this hormone in the body.
How to increase testosterone in men
For low testosterone levels, the following treatment methods can be used:
Replacement therapy. This method is rarely used. It consists of administering testosterone drugs. Testosterone can be taken into the body orally, subcutaneously, through injections, or through gels, patches and creams.
Stimulating the production of your own testosterone using various drugs. They can be either hormonal in nature or not. In particular, zinc and selenium preparations are prescribed for this purpose. Zinc is involved in testosterone synthesis, so a lack of it can cause testosterone deficiency. Selenium is also required to maintain normal testosterone levels in the body. Speroton may be prescribed as a drug with zinc and selenium.
After 2-3 weeks of treatment, testosterone levels are re-checked to ensure that the therapy is correct or if adjustments need to be made.
Diagnosis of hypogonadism
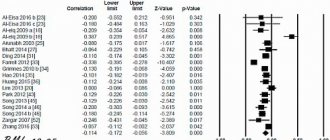
The diagnosis of hypogonadism in men is established on the basis of anamnesis, clinical picture, confirmed by laboratory and instrumental studies. Recent guidelines recommend that the diagnosis of hypogonadism should be made only in men with symptoms, external manifestations, and clearly reduced serum testosterone levels [2]. However, an analysis of the level of morning total testosterone in serum is recommended as an initial diagnostic test for hypogonadism.
Figure 2-3. Different types of hypogonadism
To calculate the level of free testosterone, you can use the online calculator www.issam.ch/freetesto.htm.
Table 2. Testosterone standards
If necessary, determine the levels of SSSH, FSH, LH, prolactin. High risk factors for developing hypogonadism:
- space-occupying formations of the hypothalamic-pituitary region;
- surgical interventions and/or radiation in the area of the sella turcica;
- long-term use of glucocorticoids, ketoconazole, opioids;
- diabetes mellitus, infertility, osteopenia and osteoporosis.
General population screening is not practical [3].
To identify a group at risk of hypogonadism, specialized questionnaires can be used.