Description of the pathology. Causes of Piriformis Syndrome
If you have pain in your buttock or thigh, or both at once, this does not mean that you have piriformis syndrome.
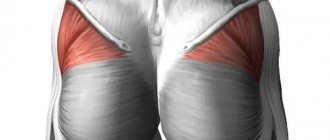
Pelvic muscles. Piriformis muscle.
A paradoxical situation has developed around piriformis syndrome. On the one hand, this syndrome is considered the most common tunnel neuropathy, everything has been well known about it for a long time, and its study is included in the basic training program for neurologists in all medical universities in the country. But, on the other hand, piriformis syndrome continues to be regularly confused with other pain syndromes of this part of the body.
By understanding the causes and mechanisms of the disease, we will understand how to eliminate it.
There is a classification that divides the causes of piriformis muscle syndrome into primary-secondary, vertebrogenic-nonvertebrogenic, local-nonlocal, etc. Without overloading you with medical terms, we will briefly and clearly describe the essence of these reasons, and below we will talk about the relationship of piriformis muscle syndrome with the spine, disc herniation and radicular syndrome.
The primary cause of piriformis syndrome is considered to be myofascial syndrome.
The secondary cause is diseases of the sacroiliac joint, gynecological, urological and proctological diseases, or, as they are also called, pelvic diseases.
Manual therapy successfully copes with both primary and secondary piriformis syndromes. However, treatment of secondary ones is, to a greater extent, the lot of specialized doctors - rheumatologists, gynecologists, urologists or proctologists. Judge for yourself. Secondary piriformis syndrome occurs against the background of long-standing pelvic pathology. The key word is “long”. During this time, the patient develops a subconscious attitude to perceive any symptom in the buttocks, pelvis or thighs as another manifestation of his illness. Therefore, he will also regard the pain of the piriformis muscle in exactly this way and, in part, he will be right. And what will he do? That's right - he will contact his attending physician - a rheumatologist, gynecologist, urologist or proctologist, and he, most likely, will also regard the pain as an exacerbation of pelvic pathology and, mechanically, will begin treatment. Fortunately, this approach, although it leaves secondary piriformis syndrome without direct treatment, often gives a positive result due to its impact on the root cause. And only when treatment of the root cause does not resolve the problem - and this happens in advanced cases of secondary piriformis syndrome - a rheumatologist, gynecologist, urologist or proctologist refer the patient to a chiropractor in order to jointly defeat the disease. This is why patients with secondary piriformis syndrome rarely see a chiropractor directly. They first turn to their “usual” doctor: a rheumatologist, gynecologist, urologist or proctologist.
Two conclusions follow from this.
- Don't start any disease. This is fraught not only with aggravation of the pathology itself, but also with the generation of new problems.
- If you do not suffer from a complex, protracted pathology of the pelvis, but at the same time, you think that your pain is piriformis syndrome, then it is not a secondary, but a primary syndrome. Therefore, you can immediately contact a chiropractor who will sort everything out. And one more thing: never diagnose yourself and do not self-medicate. Leave these issues to the doctors - this is their competence. All you need to do is find an experienced doctor.
When choosing a clinic, the main thing is to get to an experienced and knowledgeable doctor.
The primary causes of piriformis syndrome are most often myofascial syndrome.
.
Myofascial syndrome
is a condition in which small areas of tension called trigger points appear in the muscles. When these points are activated, pain occurs, which can be felt not only where the trigger point itself is located, but also in other places. This is called referred pain. In addition, myofascial syndrome suppresses muscle contractility, which is why the muscle loses its physiological properties and can itself become the cause of the next round of pathology.
Myofascial syndrome of the piriformis muscle
Causes
Myth #1 Quote from a reputable resource: “Many people believe that this (the occurrence of piriformis syndrome) occurs when the piriformis muscle goes into spasm and begins to press the nerve against the pelvic bone.” - Yes, this is definitely the reason for the pain, but the reason for the syndrome is that it caused painful contraction and inflammation in the piriformis muscle .
There are quite a few reasons for this unpleasant condition:
- Primary disruption of the piriformis muscle (eg, failure of an injection to puncture the piriformis muscle)
- Inflammatory phenomena in the hip joint (for example, with coxarthrosis)
- Diseases of the pelvic organs (genitourinary system)
- Problems in the sacroiliac joint and sacrum (injuries, neoplasms)
- Incarceration of the spinal roots of the lumbar and sacral spine
- True inflammation of the sciatic nerve (quite rare)
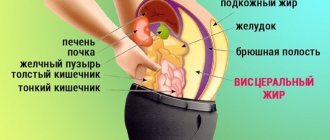
Contrary to popular belief, external factors do not have a strong influence on the piriformis muscle : it is protected from shock and low temperatures by the gluteus maximus muscle.
Symptoms and signs, diagnosis
All symptoms of piriformis muscle syndrome are divided into local symptoms and symptoms of compression of the sciatic nerve and adjacent neurovascular structures.
To understand this, it is important to pay attention to two main functions of the piriformis muscle that underlie most cases of piriformis syndrome.
The first is “pressing” the femoral head to the acetabulum of the pelvic bone (the femoral head on one side and the acetabulum on the other - this is the hip joint). When a person lies or sits, the head of his femur is not pressed against the pelvis and the hip joint is, as it were, “at neutral speed,” like a car standing still with the engine running. But as soon as a person begins to move - get up/walk - the piriformis muscle immediately turns on and tightly presses the head of the femur to the acetabulum - a “grip” occurs. Thus, the “hinge” of the hip joint comes into working condition, actively participating in raising the body to a vertical position or walking.
The function of synergy with the gluteus maximus muscle becomes most relevant when the gluteus maximus muscle, for some reason, fails. Then, having taken on a significant part of the work, the piriformis muscle begins to overload. All! Pathological processes have been started, the path to overwork of the piriformis muscle, its spasm and the further development of piriformis muscle syndrome is open. Now the occurrence of pain is only a matter of time after which a person begins to feel pain in the gluteal region.
Pain in the gluteal region can be different: pulling, aching, “braining”, aggravated by standing, squatting or walking. But, in any case, these are local symptoms.
Non-local symptoms are symptoms of compression of the sciatic nerve. To understand their mechanism, you need to know that the piriformis muscle is adjacent to the sciatic nerve.
If we look at the gluteal region layer by layer, then in the very depths are the bones and ligaments of the pelvis, on top of them lies the sciatic nerve, and above the nerve is the piriformis muscle itself. A kind of tunnel is formed in which the sciatic nerve is located between the osteoligamentous structures and the piriformis muscle.
A healthy muscle does not put pressure on the nerve. But, as soon as pathology arises, the piriformis muscle immediately begins to spasm, harden and press the nerve against the osteoligamentous structures. This is the beginning of tunnel syndrome or tunnel neuropathy. Compression of the sciatic nerve disrupts the passage of impulses through it. Which ones? Since the sciatic nerve is a mixed nerve, that is, it includes both sensory and motor fibers, pinching of the sciatic nerve leads to disruption of both sensory and motor impulses. This is manifested by symptoms of sensory impairment - “goosebumps”, “pins and needles” and numbness in the leg and motor symptoms – “cottonness”, wobbliness and weakness of the leg. Surely, you have encountered something similar when you “overstayed” your leg. But, with piriformis syndrome, such sensations are disturbing, almost without ceasing. In addition, it is difficult for a patient with a pinched sciatic nerve to stand on his heels or toes.
By the way, pain on the back of the leg, for many decades, was firmly associated with the sciatic nerve and was called sciatica or sciatica from the Latin name for the sciatic nerve - n. ischiadicus (nervus ischiadicus). Modern medicine has revised and significantly expanded ideas about the possible causes of such pain. Today, there are more than a dozen reasons why pain in the buttock and thigh area may occur. The most well-known cause, besides piriformis syndrome, is radicular syndrome, as well as myofascial syndrome of a number of muscles.
Sign up for a Piriformis muscle diagnostics
- Let's find out which syndrome causes the symptoms - piriformis, radicular or myofascial; Let's test the muscles for the presence of active and latent trigger points.
- Diagnostic duration is 30 minutes. This is a full-fledged examination, and not a 2-minute “feeling” for show.
- The diagnosis is carried out personally by Dr. Vlasenko A.A., a doctor with 30 years of experience, an expert in the treatment of myofascial and radicular syndromes.
Dr. Vlasenko Alexander Adolfovich, neurologist, manual therapy doctor
Sign up for diagnostics
Anatomy of the gluteal muscles
Each buttock contains 12 muscles and 20 ligaments. All of them form the relief of the “fifth point”. The main and largest muscles are the gluteus maximus, medius and minimus. Thanks to their coordinated work, a person is able to walk and maintain balance.
We recommend reading: How long can it take to pump up your abs: how long to exercise to get results - a week, a month, how long does it take for six-packs to appear?
Big muscle
This muscle covers almost the entire buttocks and is located in the superficial layer. It is she who is responsible for protruding the “fifth point”.
Thanks to it, the movements of the hip joints, the abduction of the legs back, and the vertical position of the body are carried out.
It is actively used by athletes of team sports - football, hockey, basketball, volleyball. This muscle is diamond-shaped and consists of coarse fibers.
Middle muscle
This muscle is located in the upper part of the buttocks, under the large muscle. Its shape resembles a triangle.
The function of this muscle is to abduct the thigh inward, outward, and to the sides. If a person stands on one leg, then the middle muscle tilts the body towards the supporting limb.
Minor muscle
We recommend reading: PROCEDOS; TOP 5 Questions to Yaroslav Soynikov
Like the previous one, it resembles a triangle in shape. Its functions are the same as those of the middle one - carrying out movements of the hips, bringing the body to the supporting limb during a stand on one leg.
When walking, contraction of the small muscle occurs, which prevents the pelvis from tilting towards the limb being carried.
Treatment methods. Which doctor treats piriformis syndrome?
An integrated approach is used in the treatment of piriformis muscle syndrome. It includes effects on all levels involved in the formation of the vicious circle of pain. Methods of local influence on altered muscle-fascial structures are of primary importance. The most successful treatment for piriformis syndrome is gentle manual therapy. A chiropractor is a doctor who treats piriformis syndrome. Gentle manual therapy includes passive muscle stretching. Compression of myofascial pain points - pressing with your fingertips on trigger points identified during diagnosis from several seconds to a minute, with a gradual increase in pressure until the pain syndrome is completely eliminated. Postisometric relaxation PIR – relaxation of muscles after their voluntary tension. If necessary, mild correction of the vertebrae. Conducting deep tissue relaxation massage, etc.
Gentle manual therapy is the basic method of treating piriformis muscle syndrome and, in the vast majority of cases, provides a full therapeutic effect. However, in advanced cases of the disease or in the presence of concomitant pathology, it is advisable to use drug treatment: non-steroidal and steroidal anti-inflammatory drugs, muscle relaxants, B vitamins, derivatives of thioctic (alpha-lipoic) acid and other neurotropic drugs, analgesics, anticonvulsants, tricyclic antidepressants, anxiolytics, etc. .
Exercise therapy is indicated during the recovery period.
When treating secondary piriformis syndrome, along with manual therapy and the methods described above, it is necessary to treat the underlying disease.
Symptoms
In approximately 70%, the gluteal-sacral area is affected first. The pain is constant, often nagging and aching. They intensify during walking, squats, and hip adduction. To reduce discomfort, the patient has to spread his legs to the sides. Over time, pain along the sciatic nerve - sciatica - is added to the symptoms. Shooting marks appear running from the foot to the buttocks. In the area where the SGM is located, pain sensitivity decreases and a burning sensation occurs.
Hypotonia of the muscles of the foot and lower leg gradually develops. With total compression of nerve fibers, “dangling foot” may develop. The main manifestations include intermittent claudication, which is a consequence of vascular compression. The same disorder leads to a decrease in leg temperature, pale skin and numbness of the fingers.
Advantages of treatment at the Spina Zdorova clinic
- Guarantee of complete and qualified treatment. The word “full” is key in our work.
- High qualifications and extensive practical experience - 30 years.
- We consider each case individually and comprehensively - no formalism.
- Synergy effect.
- Guaranteed fair treatment and fair price.
- The location is a stone's throw from the metro in the very center of Moscow.
Osteopathic treatment
Osteopathic treatment does not just act on the sore spot, but treats the entire body as a whole; the doctor “listens to the body with his hands.” All organs and systems constantly pulsate, and spasms and tensions distort the picture characteristic of the body of a healthy person. The magnitude of these pulsations is insignificant, but is accessible to the sensitive hands of an osteopath.
Having examined these micropulsations, the doctor determines the cause of the syndrome and eliminates muscle tension. Muscle tissues and ligaments are stretched and relaxed, and the doctor uses gentle movements to move organs and tissues to return them to their normal anatomical position.
Osteopathic correction of the bones, muscles and ligaments of the pelvis, as well as the lumbosacral spine, plays a special role in osteopathic treatment. Soft muscular-fascial relaxation of the Musculus piriformis quickly restores the normal state and eliminates the cause of the syndrome - compression of the sciatic nerve and blood vessels. In especially severe cases, the treatment program is supplemented with drug blockade of the brain.
Exercise therapy in the treatment program
After the acute pain syndrome is relieved, the results of osteopathic treatment are consolidated with the help of physical therapy. This allows you to avoid re-exacerbation of the syndrome. Exercises are performed under the guidance of an instructor. The program includes the implementation of special complexes aimed at strengthening: • the muscular corset of the lower back; • buttocks; • lower extremities. Work is also carried out with other parts of the musculoskeletal system.
Treatment of BMS is not aimed at relieving symptoms, but at eliminating the root cause of the syndrome. Therefore, any pain relief without treating the provoking factor is pointless. The exercises that are prescribed to patients are aimed at fully relaxing the muscular-ligamentous system, as well as activating antagonists in the movement of the lumbosacral region