- Causes
- Symptoms
- Kinds
- Degrees
- Differences between obesity in women and men
- Diagnostics
- Treatment
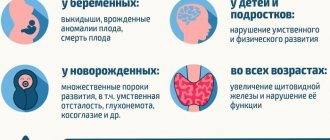
- Complications
- Prevention
- Price
Obesity is a disease that involves excessive deposition of fatty tissue, which is harmful to the human body.
Like any other disease, it requires treatment. The diagnosis of obesity is made to an adult with a body mass index equal to or greater than 30. Body mass index is calculated as the ratio of body weight to the person's height in meters squared. With a body mass index of 25 to 29, body weight is simply considered overweight. Obesity occurs when there is an energy imbalance, which occurs when the body takes in more calories than it expends. For example, if a person leads a sedentary lifestyle and eats the same amount as an active person, this leads to fat deposition and weight gain. Obesity is often promoted by high levels of insulin, genetic predisposition, disorders in the functioning of internal organs (pancreas, intestines, liver) and the endocrine system.
Obesity is a dangerous condition that leads to an increased likelihood of concomitant diseases that disrupt a person’s normal functioning.
Causes of obesity
The main reason for obesity is that unspent energy remains in the body, which is deposited in adipose tissue. This condition can occur when a person takes in more calories than they expend. But this is aggravated if a person has a genetic predisposition or diseases that contribute to excess weight gain. The following factors contribute to obesity:
- sedentary lifestyle;
- increased insulin levels;
- lack of sleep;
- stress;
- genetic predisposition;
- endocrine diseases;
- hormonal contraceptives;
- psychotropic drugs;
- disruption of the hypothalamus;
- steroid hormones;
- Prader-Willi syndrome.
These factors can cause a person to become obese.
The function of fat deposition and weight gain when consuming large amounts of calories was acquired by the body in the process of evolution, in order to expend accumulated calories during times of lack of food. In modern society, the problem of hunger has generally been solved, so it is important to monitor your body weight and, at the first signs of obesity, consult a doctor for timely treatment.
Obesity symptoms
Obesity is accompanied by the following symptoms:
- excess weight;
- dyspnea;
- nausea;
- weakness;
- drowsiness;
- decreased performance;
- swelling;
- stretch marks on the skin;
- tachycardia;
- angina pectoris;
- high blood pressure;
- constipation;
- sweating;
- joint pain;
- pain in the spine.
If you have several symptoms with a body mass index equal to or greater than 30, you should consult a doctor for diagnosis and treatment of obesity.
Childhood obesity
Childhood obesity
- one of the most pressing problems of the modern world - is the result of long-term energy imbalance, when the amount of energy consumed many times exceeds the body's needs.
Despite the certain role of genetics, the increase in the number of children suffering from obesity is associated primarily with low levels of physical activity and the predominance of junk food rich in sugars and trans fats in the diet.
Neuroendocrine disorders, congenital anomalies and chromosomal mutations fade into the background - their role in gaining excess body weight against the background of the influence of environmental factors is becoming more and more insignificant.
So, in the UK only in 2008, according to statistics, 16.8% of boys and 15.2% of girls aged 2 to 15 years had problems with excess body weight - one can imagine how these figures have changed now, 12 years later.
Obesity is associated with the development of insulin resistance, impaired glucose tolerance, and increased blood pressure, all of which contribute directly or indirectly to the development of chronic diseases. Similar to the adult body, in the child’s body the following are also noted:
- sleep apnea;
- cardiovascular pathologies;
- osteoarthritis;
- hypertension;
- depression, low self-esteem and deterioration in quality of life.
Study
: Obesity in children
Types of obesity
Types of obesity can be classified by:
- place of accumulation of adipose tissue;
- by the type of disease that causes it;
- for the reason that caused obesity.
Obesity based on the location of adipose tissue accumulation
- Visceral . In this case, fat is deposited around the internal organs. The most dangerous type of obesity, since fat negatively affects the functioning of the internal organs that surround it.
- Peripheral . Fat is deposited under the skin.
- Abdominal . In this type of obesity, fat is deposited in the abdomen, chest and shoulders, which forms an apple-shaped figure. Typically, this type of obesity develops in men. It happens both subcutaneously and can cover internal organs. It is a dangerous type of obesity, since in it fatty deposits put pressure on the abdominal cavity, disrupting the functioning of the heart, lungs, intestines and pancreas. Pressure on the heart and lungs causes hypertension and vascular disease. The risk of developing type 2 diabetes mellitus increases.
- Gynoid . In this type of obesity, fat is deposited in the lower abdomen, thighs and buttocks, creating a pear-shaped figure. In genoid obesity, fat is deposited under the skin. More common in women.
- Mixed . Fat is deposited evenly throughout the body. More common in children.
Obesity by disease type
- Cushingoid . The cause of obesity is Itsenko-Cushing's disease, in which the functioning of the hypothalamus-pituitary-adrenal glands is disrupted, due to which hormones of the adrenal cortex are produced above normal. This leads to the formation of fat deposits in various parts of the body. Mostly fat accumulates on the stomach, chest, back, shoulders and face. This obesity, coupled with Cushing's disease, leads to osteoporosis, hypertension, diabetes and osteoporosis.
- Focal . The cause of this type of obesity is lipomatosis. The disease leads to the formation of many subcutaneous benign tumors from adipose tissue.
- Hypogenital . This type of obesity is caused by a lack of the hormone testosterone in men. Lack of testosterone production may be associated with disease of the testicles, pituitary gland, congenital pathologies and other reasons. With hypogenital obesity, fat accumulates mainly in the chest, abdomen and thighs. In addition to obesity, lack of testosterone leads to underdevelopment of primary and secondary sexual characteristics in men. In women, a lack of sex hormones can also lead to obesity.
- Spongy . The cause of this type of obesity is pathology of the veins and blood vessels against the background of heart failure. This leads to fluid retention in adipose tissue and weight gain.
- Brain . This type of obesity is caused by improper functioning of the pituitary gland due to injury, disruption of the nervous system, or poisoning. At the same time, less pituitary hormones are produced, which disrupts metabolism. This disease causes fat to be deposited on the thighs, abdomen and chest.
For the reason that caused obesity
- Stress . Causes eating disorders. In a state of depression or stress, a person tends to eat a lot, eating into a negative psychological state, thereby leading the body to obesity. With psychogenic overeating, fat is deposited mainly in the abdominal area.
- Metabolic syndrome . A condition in which the metabolism of carbohydrates and fats is disrupted, resulting in excess fat being deposited.
- Heredity . Some people may have a genetic tendency to accumulate excess weight and become obese. Mutations of certain genes make it so that a person with a tendency to obesity gains weight more actively than a person without a tendency to be overweight.
- Endocrine . Disorders associated with the production of hormones, leading to obesity. Conditions may include: hypothyroidism - dysfunction of the thyroid gland; hyperprolactinemia - increased production of the hormone prolactin; hypercortisolism - increased secretion of the hormone cortisol; hypogonadism - decreased sex hormones. All these conditions lead to excess weight gain.
- Cerebral . Obesity associated with brain damage by infections, autoimmune nature, neoplasms and injuries.
- Medication . The cause of drug-induced obesity is the use of medications - steroids, hormones, cytostatics and contraceptives.
Before treating obesity, doctors conduct diagnostics to identify the causes that caused obesity. An important task for weight loss is to eliminate the diseases that led to weight gain.
Obesity in men. How to help a patient: practical advice
12.01.2020
2763
0
| E.Yu. Gritskevich , endocrinologist, andrologist (Moscow) |
During the urological Internet conference No. 6, endocrinologist, andrologist and weight loss specialist Elena Yurievna Gritskevich made a report on possible approaches to solving the problem of obesity.
According to the WHO definition, obesity is a chronic disease, heterogeneous in etiology and clinical manifestations, progressive in its natural course, characterized by excessive deposition of fat mass in the body and a relapsing nature
What is more accurate: BMI or waist circumference?
A tool for assessing the presence and severity of obesity is the body mass index (BMI) - the ratio of body weight in kilograms to the square of height in meters (kg/m2). According to WHO, a diagnosis of overweight or obesity is made in adults in the following cases:
- BMI greater than or equal to 25 – overweight;
- BMI greater than or equal to 30 – obesity;
- Waist circumference more than 94 cm.
However, it should be remembered that even with a BMI above normal, a patient can have a large percentage of muscle mass, and therefore not suffer from obesity. In some cases, focusing on waist circumference may be more reasonable.
If previously men lagged behind women in the prevalence of obesity, today its prevalence rates are almost equal between the sexes.
Patient examination algorithm
Individually, according to indications, a number of laboratory examination methods can be used in obese patients:
- performing a glucose tolerance test;
- lipid profile (total cholesterol, triglycerides, HDL, LDL);
- liver function indicators (bilirubin and its fractions, ALT, AST, alkaline phosphatase);
- determination of thyroid function (TSH, sT4);
- overnight dexamethasone test with one mg of dexamethasone if endogenous hypercortisolism is suspected;
- testosterone, prolactin, FSH, LH, estradiol, SHBG;
- C-peptide and insulin for suspected hyperinsulinemia (eg, insulinoma, nesidoblastosis, etc.).
Among the instrumental examination methods that can be used are:
- bioimpedansometry;
- Ultrasound of the abdominal organs and kidneys;
- Ultrasound of the thyroid gland;
- Ultrasound of the pelvic organs (scrotum);
- ECG;
- ECHO-KG;
- 24-hour blood pressure monitoring, ECG monitoring;
- radiography of the skull, sella turcica;
- polysomnography;
- MRI of the pituitary gland with contrast enhancement;
- MRI of the brain.
Which diet is better?
The basic principles of weight loss are a balanced diet, physical activity, normalization of carbohydrate, lipid and other types of metabolism if they are disturbed, if necessary, drug therapy, and in case of morbid obesity, bariatric surgery.
The most appropriate diet therapy for weight loss should be safe, effective and something that the patient can adhere to. Meals should include all major food groups. It is recommended to monitor the food eaten in the form of a food diary, which also records daily physical activity. Individual food preferences, eating behaviors and eating patterns must be taken into account, as well as cultural background, food traditions and availability, timing and financial concerns, food knowledge and culinary skills.
Low-calorie, fat-restricted diets lead to greater reductions in total and LDL cholesterol, while carbohydrate-restricted diets lead to greater reductions in serum triglycerides and increases in HDL cholesterol, as well as greater reductions in serum glucose HbA1c.
Separately, Elena Yuryevna mentioned the “Mediterranean” diet, which is not a specific diet, but rather a generalized term for several food options that are often found in Greece, Italy and Spain. The Mediterranean diet has the most consistent and robust scientific support for reducing the risk of atherosclerotic cardiovascular disease. There are a number of basic principles of such a diet:
- olive oil as the main source of fat;
- consumption of vegetables, legumes, whole grains, nuts and seeds;
- moderate consumption of red wine;
- moderate consumption of seafood, dairy products (cheese and yogurt), poultry and eggs;
- limiting the consumption of red meat, meat products and sweets.
You can also consider the DASH (Dietary Approach to Stop Hypertension) diet, developed by the US National Heart, Lung, and Blood Institute, mainly to correct high blood pressure. It prefers vegetables, fruits and whole grains, low-fat or low-fat dairy products , fish, poultry, lean meats, nuts, seeds and legumes, as well as fiber and minerals, particularly calcium, potassium and magnesium. Limit intake of sodium (1500–2300 mg per day), fat (no more than 27% of total daily calories), saturated fat (<6% of total daily calories), red and processed meats. Avoid sweet drinks and foods with added sugar.
The Paleolithic diet is based on the diet believed to have existed during the Paleolithic period (lasting 3.4 million years and ending 6000–2000 BC). It recommends fresh vegetables, fruits and root vegetables, grassy lean red meats, fish and seafood, eggs, nuts and seeds, and healthy oils (olive, walnut, flaxseed, macadamia, avocado and coconut). Avoid grains, legumes including peanuts, dairy products, potatoes, processed foods, refined sugar, refined oils and salt.
Optimal physical activity – how many times a week?
Physical activity is another extremely important measure in the fight against obesity. It refers to any work performed by skeletal muscles that results in energy expenditure in excess of the level characteristic of the resting state. The intensity and type of load depend on the patient, in particular, the presence of complications, and are selected individually. Moreover, any physical activity is better than no physical activity.
Dynamic (aerobic) training, performed at least 150 minutes (2.5 hours) per week of moderate activity or 75 minutes (1.25 hours) of vigorous activity, provides most of the health benefits, moderate weight loss and prevention of its increase. In the mode of 300 minutes (5 hours) per week with moderate aerobic activity or 150 minutes (2.5 hours) with intense aerobic activity, more sustainable weight loss is observed and weight regain after weight loss is prevented. If resistive (anaerobic) strength training is selected, a preliminary assessment of body composition (bioimpedance measurement) is carried out. During the training process, appropriate weight lifting techniques are used, various weights, resistance bands, etc. are used. During the recovery period, short-term muscle pain can be expected.
Medical weight correction
When managing patients with obesity, it is critical to avoid stigmatizing them while encouraging, motivating and supporting their choice to partner with their healthcare provider during treatment. From the point of view of behavioral therapy, eating disorders are divided into several types: external (I eat when I see food), emotional (I eat when I experience emotional discomfort) and restrictive (alternating strict diets with refusal of treatment). Cognitive behavioral therapy builds motivation and sets realistic goals, while patient awareness and family involvement are also important.
Several types of drugs can be used in the drug therapy of obesity:
- centrally acting drugs to accelerate saturation (sibutramine);
- drugs that affect the body's ability to absorb certain nutrients from food (orlistat);
- analogues of human glucagon-like peptide - 1 (liraglutide).
Sibutramine is a reuptake inhibitor of serotonin and norepinephrine, and, to a lesser extent, dopamine at central nervous system synapses. It accelerates the feeling of fullness, reducing the amount of food consumed, and increases the body's energy expenditure, which together leads to a negative energy balance. The drug, however, has a number of side effects: nausea, loss of appetite, constipation, dry mouth, changes in taste, headache, agitation and sweating. Contraindications include uncontrolled arterial hypertension, coronary heart disease, decompensated heart failure, heart rhythm disturbances, cerebrovascular diseases (stroke, transient cerebrovascular accident), severe liver and kidney damage. When taking the drug, blood pressure control is necessary in all patients. The drug is discontinued if the heart rate increases by more than 10 beats per minute, or the blood pressure increases by more than 10 mmHg. Art., and also if it exceeds 140/90 mm Hg. Art. with previously compensated hypertension, if shortness of breath, chest pain or joint swelling progresses. Sibutramine is also not prescribed within 14 days after taking monoamoxidase inhibitors and drugs that act on the central nervous system, including antidepressants.
Liraglutide is a glucagon-like peptide-1 receptor agonist and is an injectable drug. At low doses (1.8 mg per day) it is indicated to lower blood sugar levels in patients with type 2 diabetes. At a dose of 3 mg per day, it is approved for the treatment of obesity. Some patients may lose 5–10% of body weight, especially at higher doses of the drug. Side effects include nausea, hypoglycemia, diarrhea, constipation, vomiting, headache, decreased appetite, dyspepsia, dizziness, abdominal pain and increased lipase. Contraindicated in patients with a family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome type 2. It is recommended to discontinue therapy if pancreatitis, gallbladder disease, or suicidal behavior or thoughts are suspected. May contribute to hypoglycemia, especially in patients with diabetes mellitus receiving insulin or sulfonylureas. It can also slow down gastric emptying, which may affect the absorption of concomitantly administered oral medications.
Orlistat is a gastrointestinal lipase inhibitor that impairs the absorption of fat from food. Low doses are approved without a prescription. Some patients may lose about 5% of their body weight while taking it. Side effects include oily discharge with gas from the rectum, especially after fatty foods, which, however, can help with constipation. In addition, the drug can promote the formation of stones in the gall bladder and kidneys, and also cause malabsorption of fat-soluble vitamins (A, D, E, K). It is necessary to take a daily multivitamin against this background. Contraindications are chronic malabsorption syndrome and cholestasis. Rare cases of severe liver damage and pancreatitis have been reported. Interacts with cyclosporine, hormonal contraceptives, anticonvulsants, thyroid hormones and warfarin.
Heavy artillery
Surgical treatment is recommended for morbid obesity and ineffectiveness of previously carried out conservative measures in patients 18–60 years old.
It is carried out for BMI > 40 kg/m2 - regardless of the presence of concomitant diseases, as well as for BMI > 35 kg/m2 and the presence of severe diseases, the course of which can be influenced by reducing body weight.
A number of techniques can be used in bariatric surgery. In particular, Roux-en-Y gastric bypass provides significant improvements in metabolic disorders, but is associated with an increased risk of malabsorption complications. Promotes weight loss up to 65–75%. Has benefits for high BMI, GERD, type 2 diabetes.
Laparoscopic adjustable banding is the least invasive method and has a 25% to 40% risk of bandage cuff migration at 5 years. Provides weight reduction of 30–50%. Used for obesity without severe metabolic disorders.
Longitudinal (sleeve) gastrectomy improves metabolic diseases without disturbing the small intestinal anatomy. Micronutrient deficiencies may occur infrequently. After it, a weight loss of 50–70% is observed.
Biliopancreatic bypass provides maximum weight loss and elimination of metabolic diseases. Associated with an increased risk of deficiency of vitamins and microelements. This is the most technically complex method, providing weight reduction of up to 70–80%.
In addition, Elena Yuryevna mentioned the American BAROnova system with a silicone device TransPyloricShuttle. The intragastric system is small in size - 80–90% smaller than a balloon. It changes the passage of gastric contents by slowing gastric emptying. The effectiveness of the system was confirmed by the results of the randomized, double-blind, placebo-controlled study ENDObesity II, which involved 302 patients from nine US research centers. Approximately 67% of patients lost 5 percent or more of their body weight, and 40% lost 10% or more of their weight, compared with 14% of patients in the placebo group. Sharp fluctuations in blood pressure and other cardio-metabolic risk factors, as well as a decrease in quality of life were not observed with this treatment. Side effects included gastrointestinal events such as abdominal pain, nausea, vomiting and dyspepsia, as expected with an intragastric device designed to treat obesity through delayed gastric emptying.
Another relatively new technique is embolization of the left gastric artery. The results of the first such operations for weight loss in humans were presented in 2013. Previously, this technique was used to stop gastric bleeding. The researchers found that embolization of the left gastric artery led to a decrease in the production of the hormone ghrelin, which is involved in the regulation of hunger and satiety, which explains the decrease in body weight. The average weight loss in patients was 8–9% in the first 2–6 months after surgery and 16% in 2 years. After losing weight, the operated patients maintained it for at least a year, without any complications. The operation is performed using a microcatheter; spheres of Tris-acrylic molecules bound to gelatin molecules are used as embolization material.
In general, the choice between taking measures to change the patient’s lifestyle, as Elena Yuryevna emphasized, depends on many factors, the main ones of which are the patient’s gender, BMI, waist circumference and the presence of comorbid pathologies.
The material was prepared by V.A. Shaderkina Video of the performance can be viewed on Uro.T
The article was published in the journal “Urology Digest” No. 6-2019
Comments
To post comments you must log in or register
Obesity levels
Obesity is classified into 4 degrees:
- 1st degree . This type of obesity is diagnosed in patients with a Quetelet body mass index from 30 to 34.9 and if the weight exceeds the normal body weight by 15-29% according to the Brox formula. As a rule, patients with 1 degree of obesity have no health complaints. To treat grade 1 obesity, physical training is prescribed and the patient’s diet is adjusted. By reducing the intake of calories into the body and spending them during physical activity, the weight quickly returns to normal.
- 2nd degree . This type of obesity is diagnosed in patients with a body mass index according to Quetelet from 35 to 39.9 and if the weight exceeds the normal body weight by 30-49% according to the Brox formula. Some patients with degree 2 obesity have no health complaints, but some patients have diseases such as diabetes, hypercholesterolemia, arterial hypertension and others. To treat grade 2 obesity, lifestyle changes are prescribed: physical exercise, mental state stabilization, and regular health monitoring.
- 3rd degree . This type of obesity is diagnosed in patients with a Quetelet body mass index of 40 and if the weight exceeds the normal body weight by 50-99% according to the Brox formula. With degree 3 obesity, almost all patients experience health problems: irritability, fatigue, insomnia, erectile dysfunction, diabetes, infertility and other problems. To treat grade 3 obesity, you may need not only the help of a nutritionist and psychologist, but also an endocrinologist and a surgeon.
- 4th degree . This type of obesity is diagnosed in patients if their weight is 2-3 times higher than the normal body weight according to the Brox formula. Patients with stage 4 obesity have many health problems. Such obesity is often treated with surgical methods, including minimally invasive ones.
What is considered obesity and how does it happen?
To determine the deviation of body weight from the norm, the body mass index
– BMI. It is calculated as the ratio of body weight (in kilograms) to a person's height (in meters) squared and measured in units of kg/m².
BMI is used to characterize people aged 18 to 65 years. If the BMI is less than 18.5 kg/m², underweight is diagnosed. Normal range: from 18.5 to 24.9 kg/m². A BMI in the range of 25-29.9 kg/m² indicates the presence of overweight and obesity. This is not a disease yet, but a signal that a person should take control of his weight. With a BMI above 30 kg/m², obesity is diagnosed: from 30 to 34.9 kg/m² - I degree, from 35 to 39.9 kg/m² - II degree, over 40 kg/m² - III degree. As the degree of obesity increases, the risk of developing concomitant diseases increases - from high to extremely high, that is, concomitant diseases become simply inevitable.
There are also different types of obesity
:
Abdominal
(from the Latin word abdomen - “belly”) - when excess fatty tissue forms in the abdomen or upper torso.
This type of obesity is also called “male” obesity, since it is more common in men, or “apple” obesity. Abdominal obesity increases the risk of cardiovascular disease. Femoral-gluteal
- the lower type of obesity, more common in women. It is also called pear-shaped obesity. The lower type of obesity is often accompanied by diseases of the spine, as well as joints and veins of the lower extremities.
Mixed
when excess fat tissue is distributed evenly throughout the body.
You can determine the type of obesity by measuring your waist and hips. If a man has a ratio of waist circumference to hip circumference greater than 1.0 (WC/HR>1), then the abdominal type is diagnosed. In women, the abdominal type is established when WC/VT>0.85.
Waist circumference is also used in diagnosing obesity. If in men WC>102 cm, and in women WC>88 cm, then this is abdominal obesity. However, already with WC>94 in men and WC>80 cm in women, the risk of developing type 2 diabetes and cardiovascular diseases increases.
Obesity treatment can be carried out at the 24-hour Therapeutic Hospital on Barrikadnaya as part of the Weight Loss treatment and health program. The course of therapy can range from 1 to 10 days.
Differences between obesity in women and men
Women are more likely than men to gain excess weight, since they are genetically programmed to accumulate energy to bear a child. In women, weight gain depends on the amount of estrogen and progesterone. Hormone levels can fluctuate for various reasons, for example, depending on the phase of the menstrual cycle, as a result of which body weight can change. In women, fat accumulates mainly under the skin. At the same time, in women, fat is deposited in the form of large fat cells of a soft structure, which causes a cosmetic problem - cellulite. Women gain weight faster due to the consumption of large quantities of carbohydrates in the form of various sweets.
Men are less likely to gain excess weight. The growth of adipose tissue in men is regulated by the hormone testosterone. Low levels of the male hormone lead to excess weight gain and obesity. Testosterone levels drop after age 30, making men more likely to become overweight. Male obesity is more promoted by the consumption of fatty animal products and alcohol. In men, fat is more often deposited in the abdominal area, both under the skin and around internal organs. The structure of fat in men is denser, and the skin is tougher, so cellulite does not form.
Obesity due to psychological reasons, due to disease or due to medication does not differ between men and women.
Adipose tissue as an endocrine organ
Adipose tissue
- a source of many biologically active substances and hormones that exhibit both central and peripheral effects.
First of all, leptin is produced here - a satiety hormone, which, freely passing through the customs border of the blood-brain barrier (using a special transport system) separating nervous tissue from the circulating blood, affects the receptors of the hypothalamus - a key structure of the brain, where it reduces the production of the hormone responsible for hunger neuropeptide Y. A feeling of satiety occurs.
Interestingly, the level of this hormone differs significantly between men and women - in the former it is significantly lower, which is associated with higher concentrations of testosterone in the blood.
An increase in the amount of adipose tissue is invariably accompanied by an increase in leptin production, which entails a natural decrease in the sensitivity of cellular receptors to it - leptin resistance develops.
Study
: Obesity
Such disorders affect not only appetite dysregulation: leptin is also involved in the functioning of the reproductive system. Thus, many researchers note the cyclical nature of leptin levels, which is associated with the sequential change of conductors in a woman’s body—sex hormones. In particular, its concentration reached a maximum in the luteal phase, when this protein hormone actively stimulated the programmed death of corpus luteum cells - their apoptosis - in the absence of pregnancy.
Study
: The hormone leptin and reproduction problems
Another equally important hormone produced by fat cells is adiponectin
- also has, like leptin, a protein nature. Activation of signaling pathways leads to:
- Increased glucose utilization by skeletal muscles.
- Relaxation of smooth muscles and, as a result, a decrease in blood pressure. This effect is mediated by stimulation of endothelial cells, the inner lining of blood vessels, to produce a relaxation factor - nitric oxide.
- Prevents the division and calcification of smooth myocytes of the vascular wall, thus providing an antiatherogenic effect. In addition, it suppresses the uptake of cholesterol and its esters by cleansing cells - macrophages - which, despite the wide range of enzymes they contain, are unable to break down this organic compound and only accumulate it, turning over time into so-called “foam” cells .
- Suppression of glucose synthesis from non-carbohydrate components - inhibition of gluconeogenesis in the liver.
Study
: Metabolic effects of adiponectin
Diagnosis of obesity
Initially, obesity is determined by body mass index, as the ratio of body weight to a person’s height in meters squared. Using these calculations, the degree of obesity can be determined. Then the patient’s condition is studied in more detail and the causes of obesity are diagnosed in order to prescribe the correct treatment. For in-depth diagnosis of obesity and identification of causes, the following is carried out:
- ECG;
- Ultrasound;
- MRI;
- body composition study;
- anthropometry;
- blood pressure measurement;
- blood test;
- Analysis of urine;
- psychological analysis of the patient;
- other studies based on the patient's symptoms.
To compile a general picture of the disease, consultations with an endocrinologist, gynecologist, urologist, cardiologist, somnologist, psychologist, gastroenterologist, neurologist and other specialists may be required.
Based on the research data obtained, the nutritionist determines the patient’s condition, determines the causes of obesity and prescribes treatment aimed at eliminating the causes of obesity and weight loss.
Obesity disorders
- Hypertonic disease
- is associated, first of all, with the direct stimulation of the sympathetic nervous system by insulin, the concentration of which in the blood is many times higher than normal in people with excess body weight (its mediators, as is known, interact with the corresponding receptors on myocardial cells, increase the frequency and strength of contractions, and also have a direct effect on smooth myocytes of the vascular wall).
In addition, insulin also affects the kidneys: it promotes the retention of sodium, which drags water along with it - the volume of circulating blood increases.
With obesity, the production of angiotensinogen by adipocytes also increases - its subsequent conversion to angiotensin 2 stimulates the adrenal cortex to secrete aldosterone, a mineralocorticoid, which causes reabsorption of sodium in the renal tubules and the secretion of potassium.
In addition to this, the right atrium reduces the synthesis and release of natriuretic hormone, which helps reduce the concentration of sodium in the blood by excreting it in the urine - edema develops.
Study
: Obesity‐Related Hypertension: Pathogenesis, Cardiovascular Risk, and Treatment
- When fat is deposited in the chest and abdominal area, the mobility of the diaphragm - the main respiratory muscle - and ribs is limited, which leads to violations of ventilation of the pulmonary parenchyma
. In such patients, there is a decrease in vital capacity of the lungs, as well as a decrease in forced expiratory volume.
In addition, obesity suppresses the synthesis of the pro-inflammatory hormone adiponectin, which increases the risk of bronchial asthma.
- Disorders of carbohydrate metabolism
- in particular, the development of insulin resistance - a decisive step in the pathogenesis of type 2 diabetes mellitus. So, say, in the liver, free fatty acids prevent insulin from binding to hepatocytes, and also suppress the inhibitory effect of this hormone on gluconeogenesis (the synthesis of glucose from non-carbohydrate components).
In addition, free fatty acids have a toxic effect on the insulin-producing beta cells of the pancreas and impair the uptake and further utilization of glucose by skeletal muscle.
Study
: Obesity and insulin resistance
Obesity treatment
To treat obesity, depending on the reasons that caused it, the doctor may prescribe:
- Diet;
- Physical activity;
- Drug treatment;
- Surgical treatment of obesity;
- Help from a psychologist.
The treatment regimen for obesity is determined by a nutritionist individually for each patient. A clinically significant result of obesity treatment is considered to be a decrease in body weight by 5–10% from the initial state, an improvement in the health and well-being of the patient.
Diet
The diet is prescribed by a nutritionist based on the degree of obesity and the patient’s health status.
In general, the diet consists of excluding from the diet:
- flour;
- sweet;
- cakes and pastries;
- fatty fish, meat and sausages;
- fatty dairy products;
- salted and pickled vegetables;
- sweet drinks;
- sweet fruits;
- fried foods.
Instead of excluded foods, the diet includes:
- whole grains;
- dietary varieties of bread;
- soups;
- cereals;
- green beans and peas;
- vegetables;
- fruits.
For each patient, a nutritionist individually creates a nutrition program for the most effective weight loss.
Physical activity
The following will help increase your daily calorie expenditure:
- physical education classes;
- aerobics;
- swimming;
- cardio exercises;
- walking 10,000 steps per day;
- other physical activity.
The doctor will prescribe a list of required daily physical activity individually based on the patient’s health condition.
Drug treatment
Treatment of obesity with drugs is carried out in order to eliminate the causes that caused obesity:
- In case of hormonal imbalance, medications are prescribed that bring hormone levels back to normal.
- For inflammatory diseases of the brain, the doctor prescribes antibiotics and anti-inflammatory drugs.
- For psychological problems, antidepressants are prescribed.
- In case of eating disorders, the doctor prescribes medications that reduce appetite.
- for other health problems that lead to obesity, medications are prescribed that can eliminate these problems.
Medicines in the treatment of obesity are not used as a primary means, but as part of an individual strategy aimed at losing weight for the patient, and are aimed at treating the diseases that caused obesity.
Surgical treatment of obesity
Among the surgical methods used against obesity are:
- Liposuction;
- Stomach reduction;
- Decreased absorption capacity of the gastrointestinal tract.
Liposuction
Surgical removal of subcutaneous fat for the purpose of body contouring. The operation gives a permanent effect. Liposuction is used when other methods of combating obesity and excess weight do not provide the desired results.
The operation is performed if there are no contraindications. Liposuction is preceded by consultation with various medical specialists. The operation is performed under general anesthesia or local anesthesia.
The surgeon injects a special solution into the fat layer, makes several incisions, into which thin tubes are inserted to suck out the fat, connected to a vacuum pump. Small areas of fat can be suctioned out with large plastic syringes.
After the operation, drains are installed in the incisions, the wounds are sutured and a tight bandage is installed. After surgery, the patient follows the doctor's postoperative recommendations for faster and more successful healing and recovery.
Stomach reduction
The stomach is reduced so that the patient eats less and gets full faster, thereby losing weight. This obesity treatment measure is used when other non-surgical treatments do not work.
The surgeon reduces the stomach in one of 3 ways:
- bypass - division of the stomach with isolation of a small part and insertion into the duodenal bulb to accelerate saturation and reduce appetite for sweet and fatty foods;
- banding - dividing the stomach into two parts using a special ring;
- introduction of an intragastric balloon , replacing the volume of the stomach, using endoscopic equipment, which allows reducing the volume of food consumed. If necessary, the cylinder can be removed.
Decreased absorption capacity of the gastrointestinal tract
Effective for the treatment of obesity of 3 and 4 degrees, when other treatment methods do not work. There are 2 main methods for reducing the absorption capacity of the gastrointestinal tract:
- biliopancreatic bypass - reduction of the volume of the stomach and reconstruction of the gastrointestinal tract with diversion of bile and pancreatic juice to the terminal ileum;
- small intestinal bypass is a complex operation that excludes the small intestine from digestion.
Help from a psychologist
Consultations with a psychologist to treat the patient’s mental problems leading to obesity - depression, anxiety, apathy and others. The psychologist gives his recommendations for adjusting the patient’s lifestyle and overeating. The psychologist's advice helps change life habits in order to increase activity, reduce food consumption and improve the patient's mental state.
How to evaluate the effectiveness of obesity treatment
WHO, the World Health Organization, recommends that the effectiveness of diet and other interventions be measured based on the rate of weight loss.
If within 3 months from the start of treatment a woman has lost weight
- less than 5% of the original mass, the effect is insufficient,
- lost 5-10% of the initial weight - satisfactory,
- more than 10% is a good result.
Complications of obesity
Obesity can occur against the background of various diseases, but it can also lead to various diseases. Obesity without timely treatment can lead to complications such as:
- heart attack;
- stroke;
- type 2 diabetes mellitus;
- cholecystitis;
- gastrointestinal diseases;
- metabolic syndrome;
- joint diseases;
- depression;
- decreased reproductive function;
- cholelithiasis;
- other complications.
To avoid complications, you need to consult a doctor for help as soon as possible.
To treat obesity, you can contact our L-Med clinic by phone +7
.
Obesity prevention
In order to avoid obesity you need to:
- Monitor your weight and consult a doctor if your weight increases;
- move more;
- eat less animal fats;
- give preference to low-fat products;
- eat boiled or steamed food;
- eat less baked goods and sweets;
- reduce consumption or eliminate fried foods;
- eat more vegetables, fruits and legumes;
- eliminate hunger, eat small portions several times a day;
- do not overeat, leave the table with a slight feeling of fullness;
- half of the diet should be vegetables, a quarter - complex carbohydrates (cereals, bread), a quarter - proteins (meat, eggs and beans).
An active lifestyle and proper nutrition will help reduce the likelihood of obesity.
Cost of obesity treatment
In our clinic you can receive the following medical services:
- Liposuction (1 zone) — RUB 16,500.
- Endoscopic gastric banding for obesity - 70,000 rubles.
- Obesity surgical treatment program: bariatric surgery;
- domestic bandage - 140,000 rubles;
- imported bandage - 205,000 rubles;
- with gastric resection - 158,000 rubles.
- Appointment with a therapist—RUB 1,400.
- Appointment with an endocrinologist—RUB 1,400.
- Appointment with a cardiologist—RUB 1,400.
- Appointment with a neurologist - 1400 rubles.
- Various methods for diagnosing the disease.
You can sign up for obesity treatment at our L-Med clinic by calling +7 (4872) 302-902
or via the website.
All articles "