Candidate of Medical Sciences, leading researcher at the Federal Research Center for Nutrition and Biotechnology Svetlana Derbeneva says :
— Once upon a time, the formula of proteins-fats-carbohydrates (BJU) was considered ideal - 1:1:4. Today, experts have come to the conclusion that there is no universal ratio of proteins, carbohydrates and fats in the diet that is suitable for everyone.
The BJU formula must be constantly adjusted depending on the age, health status and needs of the person, as well as his activity.
The only constant requirement is that all three components must be present in the diet. Refusal of one of them is fraught with serious health problems.
Article on the topic
In facts and figures: protein deficiency in the diet disrupts vitamin metabolism
Bad or good?
Dividing proteins into harmful and beneficial is not entirely correct. Protein can be definitely harmful only in case of individual intolerance. Since it is proteins that trigger the cascade of allergic reactions in the body, even the most beneficial protein will be harmful to the person in whom it causes allergies. In other cases, it is more correct to talk about proteins that are more or less useful.
The value of a protein determines its composition. All proteins (and there are more than a thousand of them) consist of a long chain of amino acids, which are divided into essential (entered into the body only with food) and non-essential (they can be synthesized in the body). The more essential amino acids a protein contains, the more valuable it is.
The maximum amount of essential amino acids is contained in milk, egg, meat, fish and soy proteins. Vegetable proteins are considered less valuable. However, they have another advantage. Animal proteins enter the body in combination with not all healthy animal fat. There is no fat in plant foods. Therefore, nutritionists believe that a third of all proteins in the diet should be of plant origin.
It is believed that an adult whose work does not require serious physical activity needs 1 g of protein per 1 kg of body weight per day. In case of kidney diseases accompanied by impaired kidney function, the protein intake rate is reduced to 0.6-0.8 g per kg of body weight per day. Professional athletes have a higher protein consumption rate - 1.3-1.6 g per kg of body weight per day and even more, depending on the type of sport and sports period.
It is not advisable to exceed this norm.
Protein as medicine. What products will help cure the flu faster Read more
Nutritional therapy of phenylketonuria in stressful situations
In recent years, the issue of standard dietary therapy for phenylketonuria has received sufficient attention. Over the past 15 years, nutritional protocols for children with phenylketonuria have been developed. However, the problem of dietary therapy for phenylketonuria in stressful, unstable situations was avoided.
Often in the practice of a geneticist, there are cases when a patient, against the background of some somatic disease, infection, loss of appetite, etc., has an increase in the level of phenylalanine in the blood. Is this the result of poor nutrition? Let's try to figure out this problem. To do this, we need to remember the basics of metabolism.
The reasons for increased phenylalanine levels in phenylketonuria are:
- increased or insufficient intake of natural protein from food;
- metabolic stress: energy losses - protein catabolism;
- infections;
- somatic diseases;
- physical activity;
- loss of appetite.
In fact, all of these situations (except for the increased intake of protein from natural products into the body) come down to a lack of protein in the therapeutic mixture as a result of an increase in the body’s needs for energy and nutrients, their insufficient intake or, more simply, to “hidden starvation.” As an example, Table 1 shows the reserve indicators of substrates for the body of a child weighing 32 kg.
During short periods of “fasting,” there is a decrease in insulin levels and an increase in the secretion of glucagon and catecholamine, leading to glycogenolysis and lipolysis. Hydrolysis of triglycerides in adipose tissue releases free fatty acids and glycerol into the bloodstream, where they are transported to organs such as skeletal and cardiac muscle, kidneys and liver (a source of ketones) and used as fuel. The glucose needs of the brain and red blood cells are initially met by glycogenolysis (24 hours) and later by gluconeogenesis.
In case of “fasting” lasting more than 72 hours, insulin levels continue to decrease. There is also a decrease in glycogen reserves, while the necessary glucose is formed mainly during the process of gluconeogenesis. Due to the fact that fatty acids cannot be converted into glucose, the course of this process in the liver and kidneys depends on the supply of substrates necessary for it: amino acids from muscles, glycerol from adipose tissue and lactate obtained through anaerobic glycolysis in muscle tissue (cycle Corey). During the process of gluconeogenesis, the carbon skeleton of amino acids enters the gluconeogenic pathway, and amino groups are converted to urea and excreted daily, leading to a negative nitrogen balance and loss of up to 75 g of protein (300 g of muscle tissue). Maintaining the protein pool can be accomplished in two ways: by reducing metabolic rate by 10–15% and by reducing glucose consumption as the brain (which consumes 20% of total energy expenditure) adapts to using ketone bodies as an energy source.
So, simple fasting causes a decrease in body weight, mainly due to loss of fat, as well as a decrease in lean body mass, leading to exhaustion of the body, which can generally be characterized as a malnutrition type of marasmus. Patients with marasmus-type malnutrition have decreased energy and protein intake.
Stress fasting, called kwashiorkor, or malnutrition in the form of hypoalbuminemia, develops as a response to a combination of fasting and inflammation. It was previously thought that kwashiorkor was a result of low protein intake. However, in severe and acute inflammation, kwashiorkor may develop within a few days. In patients suffering from chronic inflammatory diseases, exhaustion develops gradually over several weeks or months. The inflammatory response is controlled by hormones and cytokines.
Currently, there is an opinion that malnutrition of the kwashiorkor type is induced in the presence of an inflammatory process in a child, who in most cases already had a malnutrition of the marasmus type.
The response to inflammation results in increased levels of adrenaline, glucagon and cortisol. These catabolic hormones lead to lipolysis, gluconeogenesis, and increased protein catabolism.
Stress hormones cause insulin resistance, resulting in hyperglycemia, hyperinsulinemia, and increased liver glucose production. In response to inflammation, cytokines such as interleukin-1 and tumor necrosis factor are synthesized. These cytokines have significant catabolic effects on body proteins. The inflammatory response to stress leads to increased energy expenditure and progressive loss of body cellular mass. Glycogen is consumed quite quickly. A small amount of protein is directly oxidized, but it serves primarily as a source of essential substrates.
Substrates released from muscle, adipose tissue, bones and other organs are recycled. These substrates are necessary for the synthesis of various protein and lipid mediators, as well as antioxidants. Amino acids resulting from the breakdown of body proteins (mainly muscle proteins) are used for the synthesis of acute phase proteins and coagulation factors for gluconeogenesis and repair processes. Glutamine and other amino acids are substrates for the immune system, intestinal mucosa and regeneration processes. At the same time, the body's utilized proteins are also an additional source of phenylalanine, leading to an increase in its level in the blood.
The paradox of the metabolic response to stress is that, being the most important adaptive reaction aimed at providing the body with the necessary substrates, stress in extreme cases can lead to impaired body functions and weight loss, and in phenylketonuria - to a worsening of the disease.
Protein synthesis and metabolism
The discovery of the general nature of the mechanism of protein synthesis is one of the great achievements of modern science, comparable to the study of outer space. The amount of protein synthesized per day depends on the body’s needs for growth, the formation of digestive and other enzymes, as well as for the replacement of proteins that have broken down in the cells of various tissues. The mucous membrane of the small intestine is renewed every one or two days. An erythrocyte lives for about 120 days. Plasma albumin is synthesized at a rate of about 10 g per day, and fibrinogen at about 2 g per day.
Protein and amino acid requirements
The estimated minimum dietary protein requirement is 0.45 g/kg body weight. In 1985, an international committee created under the auspices of the World Nutrition Council, the World Health Organization and the United Nations published new data on the safe amount of protein consumed by humans. They involve the use of essential amino acids and adequate energy supply.
It was concluded that the average adult requirement is 0.75 g of protein per 1 kg of body weight. The protein needs of other age groups were also studied. The calculation of the daily protein requirement for an infant in the first month of life is 2.5–3 g/kg; over the next 6 months this value decreases to 2 g/kg. After the first year of life, the child's needs are more difficult to determine, but they appear to gradually decrease from 2–1.8 g/kg in the first to second year of life to 0.8 g/kg for an adult. During illness and recovery, it is advisable to take 1–1.5 g/kg.
Requirements for protein and amino acids in diseases
There are two difficulties in determining protein requirements in the presence of a particular disease: different diseases affect protein requirements to varying degrees; it also depends on the severity of the disease.
With fever, fractures, burns and surgery, body protein is rapidly lost during the acute phase of the disease and must be restored during the recovery process. As a result, two problems arise: determining nutritional needs in the acute phase of the disease and determining needs during the recovery process.
Protein losses during acute illness can be significant. There are different opinions regarding high protein intake. However, there is no doubt that such losses must be made up during the recovery process.
Methods for assessing nutritional status
Anthropometry. Anthropometry reflects changes in measured anatomical parameters associated with changes in nutritional status.
Body weight is the most commonly used parameter in clinical practice, although we are still far from the ideal state of affairs when the patient has data on body weight in the epicrisis.
Body mass index (BMI). The ratio of weight to height - weight (kg) / height (mI) - is usually expressed in such a form that it allows comparison of both sexes and most age groups within the following ranges of values: 20–25 - normal nutrition; > 30 - increased nutrition; 18–20 — possible exhaustion; <18—exhaustion.
Food consumption. Formal quantification of food intake should be an integral part of the assessment of nutritional status. To do this, a food intake diary is kept by the patient or his parents for 3–7 days. The diary not only helps determine the current status, but also helps determine whether the patient's nutritional status is improving or deteriorating.
Physiological functions are impaired in malnourished patients. Such patients are at high risk of complications and unfavorable outcome of the disease. In addition, the disease itself predisposes to the development of malnutrition (Fig.).
Functional tests for immune function. Chandra showed a strong relationship between tests that reflect the state of cellular immunity and the degree of malnutrition. Lymphocyte counts of 900–1500 cells/mmI indicate moderate malnutrition, and values <900 cells/mmI indicate severe malnutrition. The proportion and number of T lymphocytes in the peripheral blood are also reduced in cases of malnutrition. Leukocyte function, antibody secretion, and complement levels may be impaired.
Laboratory parameters. The main parameter for patients with phenylketonuria remains the level of phenylalanine in peripheral blood.
Serum albumin reflects the severity of inflammatory disease, injury, etc., rather than the degree of malnutrition, although a delayed return of serum albumin to normal values after the acute phase of the disease may be a consequence of inadequate dietary protein and energy intake.
Proteins with a shorter half-life, prealbumin (2 days) and transferrin (7 days), as well as albumin, are strongly influenced by redistribution and dilution, but they are more reflective of nutritional status.
Summarizing the above, let's try to determine the tactics of a doctor - a geneticist in a situation of hypercatabolism (increased protein and energy consumption) in a child with phenylketonuria.
With any illness, increased physical activity, loss of appetite (for example, against the background of acute respiratory viral infection), the child does not receive enough protein and energy. Glycogen reserves are low. The most accessible source of protein is skeletal muscle (in more serious situations, the intestines and then internal organs begin to suffer). The result of catabolism is an increase in phenylalanine levels in peripheral blood tests.
A simple, logical solution would be to increase energy and protein support. Protein requirements during the period of illness and recovery increase by 1–1.5 g/kg body weight. Thus, the child should receive an additional 20–50 g of dietary protein. At the same time, it is necessary to temporarily reduce the consumption of natural protein by 20–50% until phenylalanine levels normalize.
The most capacious energy substrate is fats. When 1 g of fat is metabolized, 9 kcal of energy is released. The second most important source of energy is carbohydrates - when metabolizing 1 g of carbohydrates, 4 kcal are released. Against the background of the disease, the child should receive an additional 10–15 kcal/kg in addition to the age norm of basic energy.
The distribution of energy among nutrients in diet therapy is carried out in the following proportions: proteins - 10-15%, fats - 35-40% and carbohydrates - 45-55%.
Let us give an approximate calculation of nutrition for a child with phenylketonuria against the background of a hypercatabolic state.
Child 5 years old, ~ 20 kg, peripheral blood phenylalanine level - 10 mg%, MD mil PKU-1 (1 can 400 g):
- phenylalanine/day - 300 mg;
- protein of natural products - 300: 50 = 6 g - 2 g = 4 g;
- required amount of protein per day + 1 g/kg body weight per day during the period of illness and recovery - 30 g + 20 g = 50 g;
- the required amount of protein of a special formula is 46 g;
- formula volume per day - 100 g MD mil PKU-1 - 20 g protein; 230 g MD mil PKU-1 - 46 g protein;
- daily caloric intake + 15 kcal/kg body weight per day during the period of illness and recovery - 1700 kcal + 300 kcal = 2000 kcal;
- energy distribution: proteins - 10% - 200 kcal (50 g); fats - 35% - 805 kcal (89 g); carbohydrates - 55% - 1100 kcal (275 g).
Child 12 years old, ~ 46 kg, peripheral blood phenylalanine level - 15 mg%, MD mil PKU-3 (1 jar 400 g):
- phenylalanine / day - 400 mg;
- protein of natural products - 400: 50 = 8 g - 3 g = 5 g;
- required amount of protein per day - 45 g + 46 g = 91 g;
- the required amount of protein of a special formula is 86 g;
- formula volume per day - 100 g MD mil PKU-3 - 69.1 g protein; 124.5 g MD mil PKU-3 - 86 g protein;
- daily caloric intake + 15 kcal/kg body weight per day during the period of illness and recovery - 2500 kcal + 460 kcal = 2960 kcal;
- energy distribution: proteins - 12% - 364 kcal (91 g); fats - 35% - 1036 kcal (115 g); carbohydrates - 53% - 1570 kcal (392 g).
Despite the fact that today doctors have the necessary techniques to determine the needs of a child with phenylketonuria, a certain gap between knowledge and practice remains, which entails negative clinical and economic consequences. Professionals should keep in mind that constant monitoring of nutritional support for phenylketonuria is necessary to ensure that the child is provided with adequate nutrition.
E. V. Denisenkova E. P. Klykova , Candidate of Medical Sciences Center for Neonatal Screening of the Russian Federation, Children's Psychiatric Hospital No. 6, Moscow
Saturated or unsaturated?
Healthy unsaturated fats (found in olive oil, nuts, avocados and fish), on the other hand, protect the heart by lowering bad cholesterol and increasing good cholesterol. The most valuable component of unsaturated fats is omega-3 and omega-6 unsaturated fatty acids. The record holders for their content are fish and olive oil. They resist the formation of blood clots and cholesterol plaques, improve brain function, strengthen memory and immunity. According to some studies, consuming these acids can reduce the risk of heart disease by 35%, and the chance of dying from a heart attack by 50%. The norms for fat consumption for a person happy with his figure are 0.8-1 g per 1 kg of body weight per day.
By the way!
A lack of fat immediately affects your appearance - the skin wrinkles and dries out, hair becomes lifeless, and nails become brittle. In addition, fats supply the body with energy, regulate heat exchange and promote the absorption of many other useful substances. Provided that the diet contains the right fats. Harmful fats include saturated fats, which are found in full-fat dairy products, meat, processed meats and fast food. They provoke the deposition of cholesterol plaques on the walls of blood vessels and, as a result, heart disease.
Kills the liver, destroys the brain. What are the dangers of a high-fat diet? Read more
Minimum amount of protein in the diet
An approximate calculation can show how much protein our body needs to renew existing tissues. The cells of all muscle tissue are completely renewed in 16 years at an average weight. For a weight of 80 kilograms in an athletic person, we have a muscle mass of approximately 45 kg, and 20% of this mass is 9000 g of protein, the regeneration of which requires that our body synthesize a minimum of 1.5 g of protein per day. In addition to replacing aging muscle cells, such as when exercising, additional protein will be needed to restore the integrity of damaged muscle fibers.
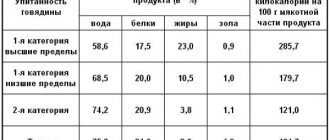
Table from the book of Zbarsky B.I. "Biological chemistry "
Table No. 2. Ratio of NAC to total protein in food
The table shows the ratio of NAC to other amino acids in foods.
For normal muscle growth for a training athlete, protein intake should naturally be higher than the minimum values mentioned. At the same time, there are limits to metabolic processes and there are a number of studies suggesting that consumption of more than 1.6 grams per kilogram of body weight per day (in absolute terms, this is 128 grams for an 80 kg person) does not produce muscle gain in training athletes.
Table No. 3. Ratio of NAC to product cost
According to WHO, the minimum value of NAC, in absolute value equal to 14.7 grams for a person weighing 80 kg or 100% of the daily value of a complete amino acid profile for a person weighing 80 kg, can be obtained from the following foods:
The values in this table may be misleading because they are based on the consumption of one food item. If you combine different foods , you will get a more complete diet.
For example , 200 grams of buckwheat grains (dry weight) and 200 grams of tofu will have 100% amino acid profile. Since (Methionine + Cysteine) in 200 grams of tofu there is only 26% of the daily value for a person weighing 80 kg , and in 200 grams of buckwheat there are 66% of the daily value (Methionine and Cysteine).
Carbohydrates
Everyone knows that carbohydrates are the enemies of your figure. Therefore, as soon as there is an urgent need to lose weight, the first step is usually to give up carbohydrates. And they make a serious mistake. With a prolonged lack of carbohydrates, the body cannot completely burn fat, which is why it forms metabolic byproducts - ketones. Accumulating in the blood and urine, they cause an unpleasant state - ketosis, the symptoms of which are lethargy, fatigue, irritability, and decreased performance. Therefore, a carbohydrate-free diet is considered one of the hardest for the body.
It is no coincidence that carbohydrates are included in the triad of essential nutritional components: they provide the body with energy, nourish the brain and are responsible for the feeling of fullness. The main thing is to eat the right carbohydrates.
These organic compounds have different structures.
Article on the topic
Buns as opiates. How do carbohydrates affect our brain?
Simple or complex?
Simple (easily digestible) carbohydrates, which are also called fast carbohydrates for their ability to instantly increase blood sugar levels. The body can extinguish this surge in only one way - by turning sugar into fat deposits. In addition, to process large amounts of sugar, large amounts of insulin are required. Eating fast carbohydrates wears out the pancreas, so it is better to minimize their amount in the diet.
Another thing is complex carbohydrates, which consist of hundreds of different elements. They release energy gradually, providing long-lasting saturation. Such carbohydrates per day must be consumed at least 50-55% of the total calories - 3 g per kilogram of weight. And if a person is engaged in physical labor or is actively involved in sports, then the rate of carbohydrate consumption should be increased at the rate of 5-6 g per kilogram of weight.
Complex carbohydrates are found in vegetables, fruits, cereals and whole grain bread. Fast carbohydrates - baked goods and sweets.
How not to eat harmful things? Learning to choose healthy products Read more
Why the correct ratio of BZHU is so important for weight loss↑
The correct ratio of BZHU is very important for the body. By changing this ratio, you can productively adjust your weight up or down, build muscle more efficiently, “accelerate” your metabolism, or reduce body weight.
Diets don't work
It’s no wonder that “diet exhaustion” has become a commonly used phrase. Almost all “fast” diets involve avoiding fat consumption and reducing the amount of carbohydrates in the diet. Despite the apparent effect and several kilograms lost, this is a huge stress for the body. The body enters “economy mode” and is very reluctant to get rid of accumulated fat deposits, immediately compensating for losses with any excess received. As soon as the diet is finished, the kilograms that were lost will return with gain.
How to find out your norm?
There are no universal nutritional standards. Any numbers that are given in textbooks on dietetics and in books on proper nutrition are averaged data. In practice, the daily requirement for proteins, fats and carbohydrates varies depending on the person’s activity level, his goal, body type, the presence of diseases affecting metabolism, region of residence, and so on.
The calculation of calorie intake can be found using the Harris-Benedict formula, which showed that the number of calories a person needs every day depends on the basal metabolic rate (BMR) and active metabolic rate (AMR).
Article on the topic
Gender, weight and age. How many calories do you need per day?
How to calculate your daily calorie intake?
Calorie intake depends on many factors and will be different for each person. Of course, sometimes nutrition consultants resort to averages or use data obtained by weighing a client on a body composition analyzer scale. However, if you want the menu you have compiled to be truly individual and accurate, then it is better to use the appropriate formula.
To calculate, you need to know the weight, height, gender and age of the person for whom the daily caloric intake is determined, as well as the level of physical activity. Much depends on the last indicator, since people leading an active lifestyle require more energy to function.
Don’t forget about the ambient temperature: the basic calorie intake is calculated taking into account comfortable temperature conditions; in cold weather, the energy value of food can be slightly increased, and in hot weather, on the contrary, reduced (by about 10%).
Now let's move directly to the formula for calculating the daily calorie requirement (DC):
SPK = (BOOV + SDDP) × KFA
Let's decipher the abbreviation:
- DAC – daily calorie requirement;
- BOOV – basal metabolic rate;
- SDDP – specific dynamic effect of food;
- KFA – physical activity coefficient.
Is it more convenient to get information about calculating calorie intake from a video? Then watch how to calculate the SPC in a video lecture from a sports medicine doctor and an expert at our school of nutritionists, Yuri Butria:
To make calculations using this formula, you must first find out all the quantities present in it:
Basal metabolic rate (BMR)
This is the amount of energy that the body requires to function in comfortable temperature conditions and a calm state. This indicator depends on the weight, height, gender and age of the client. As you know, men have a slightly higher basal metabolism than women, so the formulas for both sexes are also different.
To calculate BOOB, we recommend using the Mifflin-San Geor formula, the most common among nutritionists. It looks like this:
MIFFLIN-ST JEORA FORMULA
FOR WOMEN: BOOV = 9.99*WEIGHT (KG) + 6.25*HEIGHT (CM) – 4.92*AGE (YEAR) – 161
FOR MEN: BOOV = 9.99*WEIGHT (KG) + 6.25*HEIGHT (CM) -4.92*AGE (YEAR) + 5
Carefully plug all the values into the above formula and get the client's basal metabolic rate.
Specific dynamic action of food (SDAF)
This is the amount of energy that the human body needs to chew and digest the food eaten, as well as to transport nutrients from it.
As a rule, this indicator is 10% of the basal metabolism, so it is very easy to calculate it using this simple formula: ADDP = 10% * BOOV
Physical Activity Quotient (PFA)
It is clear that the level of physical activity may be different every day, but only because of this no one will constantly recalculate the daily calorie requirement. So, when determining this indicator, you should rely on the average result and use the already developed CFA table (at our school of nutritionists we carry out calculations using the same table):
TABLE OF PHYSICAL ACTIVITY RATIOS
| Minimal physical activity (sedentary work) | 1,2-1,3 |
| Light daily activity or light exercise 1-3 times a week | 1,4-1,5 |
| Workout in the fitness room 4-5 times a week or moderate work | 1,6-1,7 |
| Intense training 4-5 times a week | 1,8-1,9 |
| Daily workouts | 2-2,1 |
| Daily intense workouts or regular workouts 2 times a day | 2,2-2,3 |
| Intense training 2 times a day or heavy physical work | 2,4-2,5 |
Now calculate each indicator separately and substitute them into the general formula for calculating the daily calorie requirement (DC). Remember that the result shows how much energy the client’s body needs every day. If you stick to it, your weight will stabilize, since the intake of calories from food will correspond to their expenditure.